Also see:
Sugar Ads
Polyunsaturating America: Mazola’s Marketing
Gelatin, stress, longevity
Gelatin > Whey
Thyroid peroxidase activity is inhibited by amino acids
Whey, Tryptophan, & Serotonin
Tryptophan, Fatigue, Training, and Performance
Carbohydrate Lowers Free Tryptophan
Protective Glycine
Enzyme to Know: Tryptophan Hydroxylase
Tryptophan Metabolism: Effects of Progesterone, Estrogen, and PUFA
Intestinal Serotonin and Bone Loss
Serotonin and Melatonin Lower Progesterone
Role of Serotonin in Preeclampsia
Maternal Ingestion of Tryptophan and Cancer in Female Offspring
Melatonin Lowers Body Temperature
Serotonin, Fatigue, Training, and Performance
Gelatin, Glycine, and Metabolism
Omega -3 “Deficiency” Decreases Serotonin Producing Enzyme
Hypothyroidism and Serotonin
Estrogen Increases Serotonin
10 Tips for Better Sleep
Gelatin Ads
Posted in General.
Comments Off on Gelatin Ads
– March 28, 2013
Granulated Sugar as Healer
Also see:
Theurapeutic Honey – Cancer and Wound Healing
Wound Healing: Topical Omega -9 is Superior to the “Essential Fatty Acids”
Sugar (Sucrose) Restrains the Stress Response
Thumbs Up: Fructose
The Sugar Cure
“Applying glucose and insulin topically to the wound, it heals quickly. The very old practice of treating deep wounds with honey or granulated sugar has been studied in controlled situations, including the treatment of diabetic ulcers, infected deep wounds following heart surgery, and wounds of lepers. The treatment eradicates bacterial infections better than some antiseptics, and accelerates healing without scarring, or with minimal scarring. The sugar regulates the communication between cells, and optimizes the synthesis of collagen and extracellular matrix.” -Ray Peat, PhD
J Wound Care. 2002 Feb;11(2):53-5.
Why do some cavity wounds treated with honey or sugar paste heal without scarring?
Topham J.
As well as having antimicrobial properties, honey and sugar paste are associated with scarless healing in some cavity wounds. This article uses evidence to suggest why these products can modify excessive collagen production to prevent scarring.
J Tissue Viability. 2000 Jul;10(3):86-9.
Sugar for wounds.
Topham J.
Sugar in its pure form, or incorporated into a paste containing an adhesive hydropolymer (gum), is a non-toxic treatment for a variety of wounds. Not only does it provide a suitable clean environment for angiogenesis to take place, but it will debride the wound surface and reduce odour. The presence of an adhesive hydropolymer seems to prevent hypergranulation, scarring and contraction.
Lancet. 1985 Jul 27;2(8448):180-4.
Use of granulated sugar in treatment of open mediastinitis after cardiac surgery.
Trouillet JL, Chastre J, Fagon JY, Pierre J, Domart Y, Gibert C.
19 critically ill adults with acute mediastinitis after cardiac surgery were treated with granulated sugar, either directly (11 patients) or after failure of continuous irrigation (8 patients). Mediastinal tissue cultures were positive in 18 patients. Packing the mediastinal cavity with granulated sugar every 3 or 4 h resulted in near-complete debridement of the wound and rapid formation of granulation tissue in all patients and sterilisation of the wound after an average of 7.6 days. Dressings were easy and painless to change. 5/19 (26%) patients died before discharge, but none because of wound complications. The rest were discharged on average 54.2 days (range 29-120) after initial debridement of the wound; 11 underwent secondary surgical closure of the wound and in 3 the wound healed by granulation tissue formation alone. No recurrence of sternal infection has occurred after a mean follow-up of 8.2 months (range 3 to 17).
N Engl J Med 2011; 364:1855May 12, 2011DOI: 10.1056/NEJMicm1012908
Sugar to Reduce a Prolapsed Ileostomy
Alexandra R.M.L. Brandt, M.D., and Olaf Schouten, M.D., Ph.D.
A 62-year-old man presented to the emergency department with a prolapsed ileostomy (Panel A). He had undergone ileostomy 25 months earlier for the treatment of mesenteric ischemia requiring an extended right hemicolectomy. The prolapse had occurred 12 hours before presentation, with no known cause. An attempt at manual reduction of the prolapse was unsuccessful. The patient’s severe coexisting cardiovascular and respiratory conditions made the use of general anesthesia and surgical reduction a risky therapeutic option. As has been previously described in the management of anal prolapse, bovine uterine prolapse, and (rarely) ileostomal prolapse, plain granulated sugar was applied to the mucosa of the prolapsed ileum to promote the osmotic shift of fluid out of the edematous tissue (Panel B). Within 2 minutes, the edema had diminished sufficiently to allow spontaneous reduction of the prolapsed ileum (Panel C). Twenty-four hours later, endoscopic evaluation revealed mild ischemia of the lower portion of the ileum, which required no treatment. The patient was discharged the following day. Ileostomal prolapse did not recur during 6 months of follow-up.
Orv Hetil. 1990 Apr 1;131(13):691-5.
[Topical treatment using granulated sugar in advanced mediastinitis following open heart surgery].
[Article in Hungarian]
Szerafin T, Vaszily M, Péterffy A.
The complications caused by infection were examined prospectively in the case of 1164 patients who had undergone open heart operation. Postoperative mediastinitis occurred in 15 cases (1.3%). Owing to mediastinal infection verified by bacteriological findings all patients had to undergo surgical intervention. Ten patients were treated by closed mediastinal irrigation. This method was effective in the case of five patients. Granulated sugar treatment was locally applied in five cases because of an infection, relapsing in spite of a closed treatment, and in four cases primarily, because of advanced mediastinitis and sternum osteomyelitis. With the mediastinal cavity being filled with granulated sugar twice a day, a rapid emptying of the wound and granulation tissue formation was observed in all patients. Redressing was easy and painless. Out of the 9 patients treated by granulated sugar three died before being discharged, but none of the deaths were due to wound complications. The rest of the patients were discharged cured averagely after 91.6 +/- 8.0 days. During the average 22 months’ follow up period recurrence of sternal infection was not observed in the group treated by granulated sugar, while out of the 5 patients cured by closed mediastinal irrigation two had to undergo another operation after a few months because of the formation of sternal fistula. The authors consider the granulated sugar treatment to be an effective method in the treatment of obstinate and advanced mediastinal infections.
J Cardiovasc Surg (Torino). 2000 Oct;41(5):715-9.
Treatment of recurrent postoperative mediastinitis with granulated sugar.
De Feo M, Gregorio R, Renzulli A, Ismeno G, Romano GP, Cotrufo M.
BACKGROUND:
The authors report their experience with granulated sugar as dressing technique in the treatment of postoperative mediastinitis refractory to a closed irrigation system.
METHODS:
Between January 1990 and January 1998, mediastinitis developed in 61 (0,93%) of 6521 patients who had undergone open heart surgery. Diagnosis of sternal infections was based on wound tenderness, drainage, cellulitis, fever associated with sternal instability. All of them were initially treated with surgical debridement and closed chest irrigation. Nine patients with postcardiotomy mediastinitis refractory to closed chest irrigation underwent open dressing with granulated sugar. All of them were febrile with leukocytosis and positive wound cultures.
RESULTS:
Bacteria isolated were staphylococcus aureus in 6 cases, staphylococcus epidermidis in 2 and pseudomonas in 1. Redebridement was performed in all cases and the wound was filled with granulated sugar four times a day. Fever ceased within 4.3+/-1.3 days from the beginning of treatment and WBC became normal after 6.6+/-1.6 days. Three patients had hyperbaric therapy as associated treatment. Complete wound healing was achieved in 58.8+/-32.9 days (three patients underwent successful pectoralis muscle flaps).
CONCLUSIONS:
Sugar treatment is a reasonable and effective option in patients with mediastinitis refractory to closed irrigation treatment. It may be used either as primary treatment or as a bridge to pectoralis muscle flaps.
Scand J Thorac Cardiovasc Surg. 1991;25(1):77-80.
Granulated sugar treatment of severe mediastinitis after open-heart surgery.
Szerafin T, Vaszily M, Péterffy A.
Fifteen cases of mediastinitis developing after 1,164 open-heart operations (incidence 1.3%) were analyzed. Closed mediastinal irrigation was used as primary therapy in ten cases and led to complete healing in five. Granulated sugar treatment was given primarily to four patients and to five others after failure of closed mediastinal irrigation. The sugar treatment was successful in six patients with hospital stay averaging 91.6 +/- 8 days. The three other patients in this group died before discharge from hospital. During 22-month follow-up there was no recurrence of mediastinitis in the granulated sugar group, but reoperation was necessitated by sternal fistula in two of the patients with closed mediastinal irrigation. Granulated sugar treatment is effective in refractory, severe mediastinal infections.
South Med J. 1981 Nov;74(11):1329-35.
Use of sugar and povidone-iodine to enhance wound healing: five year’s experience.
Knutson RA, Merbitz LA, Creekmore MA, Snipes HG.
Over a 56-month period (January 1976 to August 1980), we treated 605 patients for wounds, burns, and ulcers with granulated sugar and povidone-iodine. Rapid healing ensued, due to a reduction in bacterial contamination, rapid debridement of eschar, probable nourishment of surface cells, filling of defects with granulation tissue, and covering of granulation tissue with epithelium. The requirements for skin grafting and antibiotics were greatly reduced, as were hospital costs for wound, burn, and ulcer care.
BMJ Case Rep. 2013 Feb 28;2013. pii: bcr2012007565. doi: 10.1136/bcr-2012-007565.
Granulated sugar to reduce an incarcerated prolapsed defunctioning ileostomy.
Mohammed O, West M, Chandrasekar R.
This case report discusses the successful application of granulated sugar to reduce a prolapsed ileostomy thereby eliminating the need for an emergency surgery.
Tech Coloproctol. 2010 Sep;14(3):269-71. doi: 10.1007/s10151-009-0507-1. Epub 2009 Jul 11.
Reduction of an incarcerated, prolapsed ileostomy with the assistance of sugar as a desiccant.
Shapiro R, Chin EH, Steinhagen RM.
Prolapse is a well-described complication after ileostomy or colostomy, and is typically asymptomatic and easily reduced. Acute incarceration of a prolapsed stoma is a rare event, however. A patient presented with an incarcerated, prolapsed ileostomy causing small bowel obstruction and stomal ischemia. Successful reduction was performed with the assistance of sugar as a desiccant. Incarceration of a prolapsed ileostomy is highly atypical, but can be approached in a similar manner to an incarcerated rectal prolapse. Successful reduction can prevent an emergent operation, allowing for medical optimization and elective surgical treatment if necessary.
J Diabetes Sci Technol. 2010 Sep 1;4(5):1139-45.
Use of sugar on the healing of diabetic ulcers: a review.
Biswas A, Bharara M, Hurst C, Gruessner R, Armstrong D, Rilo H.
With the advent of several innovative wound care management tools, the choice of products and treatment modalities available to clinicians continues to expand. High costs associated with wound care, especially diabetic foot wounds, make it important for clinician scientists to research alternative therapies and optimally incorporate them into wound care protocols appropriately. This article reviews using sugar as a treatment option in diabetic foot care and provides a guide to its appropriate use in healing foot ulcers. In addition to a clinical case study, the physiological significance and advantages of sugar are discussed.
J Exp Pathol (Oxford). 1990 Apr;71(2):155-70.
A controlled model of moist wound healing: comparison between semi-permeable film, antiseptics and sugar paste.
Archer HG, Barnett S, Irving S, Middleton KR, Seal DV.
An established wound model in the pig has been modified using a Stomahesive ring to enable study of the effects of fluids used in wound care. Full thickness wounds (up to 9 mm deep) were treated with the substances under test. Each application was held in place with a Stomahesive flange, the inner part of which had been excised as far as the hard plastic ring. All dressings were then covered with OpSite which allowed gaseous exchange whilst retaining treatment fluids and secretions. Wounds were treated immediately and at 2 and 4 days. The experiment was terminated after 7 days and the whole wound, with dressing, was excised for histological examination. The wounds covered with OpSite alone and those treated with sugar paste under Opsite were found to be infilled with granulation tissue over which epidermal migration was taking place. Those wounds which had been packed with gauze, to which had been added one of the following: chlorhexidine gluconate 0.2%, Irgasan 0.2%, povidone iodine 0.8% or EUSOL half-strength, showed delayed healing in that less infilling had taken place over the same time period. This delay could be attributed to the nature of the chemicals used and/or the influence of gauze packing. This delay in the healing of wounds treated with chemical agents was least with EUSOL half-strength and greatest with chlorhexidine. No toxic effects were observed with sugar paste which may be preferable to antiseptics for the management of dirty or infected wounds.
Pathogenesis of Wound and Biomaterial-Associated Infections 1990, pp 159-162
Development of a Semi-Synthetic Sugar Paste for Promoting Healing of Infected Wounds
Keith R. Middleton, David V. Seal
Pastes comprising primarily sucrose and polyethylene glycol 400 have been used with good effect to treat infected and malodorous wounds in many patients. The pastes have good in vitro antimicrobial activity and demonstrated no toxic effects in full thickness wounds in a controlled trial in a pig model. Other commonly used antiseptics that were tested showed impairment of wound healing. Sugar paste is inexpensive and should be considered for the treatment of infected wounds in preference to other antiseptics.
Ann Emerg Med. 1997 Sep;30(3):347-9.
Sucrose as an aid to manual reduction of incarcerated rectal prolapse.
Coburn WM 3rd, Russell MA, Hofstetter WL.
Incarcerated rectal prolapse is a potential surgical emergency. We report a case in which a simple but effective technique involving the desiccating effect of granulated sugar (sucrose) was used to aid the manual reduction of prolapsed but viable rectal tissue.
Dis Colon Rectum. 1991 May;34(5):416-8.
Sugar in the reduction of incarcerated prolapsed bowel. Report of two cases.
Myers JO, Rothenberger DA.
Incarcerated, prolapsed rectum, colostomies, and ileostomies, when viable, may be reduced using ordinary table sugar. The placing of sugar granules on the incarcerated bowel results in a decrease in tissue edema and spontaneous bowel reduction. The technique, case reports, and a review of the literature are herein reported.
J Wound Care. 2011 May;20(5):206, 208, 210 passim.
Use of granulated sugar therapy in the management of sloughy or necrotic wounds: a pilot study.
Murandu M, Webber MA, Simms MH, Dealey C.
” Preliminary data suggest that sugar is an effective wound cleansing and is safe to use in patients with insulin-dependent diabetes. In vitro studies demonstrate that sugar inhibits bacterial growth.”
Microb Pathog. 2012 Jan;52(1):85-91. doi: 10.1016/j.micpath.2011.10.008. Epub 2011 Nov 4.
Sugar inhibits the production of the toxins that trigger clostridial gas gangrene.
Méndez MB, Goñi A, Ramirez W, Grau RR.
“The present results are analyzed in the context of the role of CcpA for the development and aggressiveness of clostridial gas gangrene and the well-known, although poorly understood, anti-infective and wound healing effects of sugars and related substances.”
Arch Dermatol Res. 2007 Nov;299(9):449-56. Epub 2007 Aug 7.
Mixture of sugar and povidone-iodine stimulates healing of MRSA-infected skin ulcers on db/db mice.
Shi CM, Nakao H, Yamazaki M, Tsuboi R, Ogawa H.
“These results indicate that wounding on db/db mice provides a useful animal model of bacterial skin infections, and that a 70% sugar and 3% povidone-iodine paste is an effective topical agent for the treatment of diabetic skin ulcers.”
Arch Dermatol Res. 2006 Sep;298(4):175-82. Epub 2006 Jul 22.
Mixture of sugar and povidone–iodine stimulates wound healing by activating keratinocytes and fibroblast functions.
Nakao H, Yamazaki M, Tsuboi R, Ogawa H.
“SP, the mixture of sugar and povidone–iodine, is likely to act on wounds not only as an antibiotic agent, but also as a modulator for keratinocytes and fibroblasts.”
Antimicrob Agents Chemother. 1983 May;23(5):766-73.
In vitro study of bacterial growth inhibition in concentrated sugar solutions: microbiological basis for the use of sugar in treating infected wounds.
Chirife J, Herszage L, Joseph A, Kohn ES.
The use of sugar for the treatment of infected wounds was investigated in in vitro experiments with bacteria pathogenic to humans, such as Escherichia coli, Pseudomonas aeruginosa, Klebsiella pneumoniae, and Staphylococcus aureus. Studies showed that solutions of appropriate sugar concentration incubated at pH 7.0 and 35 degrees C were lethal to the bacterial species studied. On the basis of these results, it is proposed that an important function of sugar in the treatment of infected wounds is to create an environment of low water activity (aw), which inhibits or stresses bacterial growth.
Int Surg. 1984 Oct-Dec;69(4):308.
Sugar in the treatment of infected surgical wounds.
Rahal F, Mimica IM, Pereira V, Athié E.
Forty-two patients with infected wounds were treated with common sugar. In all cases, the infections cleared within five to 30 days.
More:
Merck Veterinary Manual: Initial Wound Treatment
“Sugar Dressings
Sugar has been used as an inexpensive wound dressing for over 3 centuries. The use of sugar is based on its high osmolality, which draws fluid out of the wound. Reducing water in the wound inhibits the growth of bacteria. The use of sugar also aids in the debridement of necrotic tissue, while preserving viable tissue. Granulated sugar is placed into the wound cavity in a layer 1-cm thick and covered with a thick dressing to absorb fluid drawn from the wound. The sugar dressing should be changed once or twice daily or more frequently as needed (eg, whenever “strike-through” is seen on the bandage). During the bandage change, the wound should be liberally lavaged with warm saline or tap water. Sugar dressings may be used until granulation tissue is seen. Once all infection is resolved, the wound may be closed or allowed to epithelize. Because a large volume of fluid can be removed from the wound, the patient’s hemodynamic and hydration status must be monitored and treated accordingly. Hypovolemia and low colloid osmotic pressure are complications that may be associated with this therapy.”
The combination of sugar with antibiotics may hold hope for treatment of persistent bacterial infections
Sweet Blood: A back country treatment for open wounds
Sugar application in reduction of incarcerated prolapsed rectum
Trick of the Trade: “Pour some sugar on me”
A spoonful of sugar helps wounds heal faster
Sugar heals wounds faster than antibiotics
The use of granulated sugar to treat two pressure ulcers
Pouring granulated sugar on wounds ‘can heal them faster than antibiotics’
Family sugar remedy tested for healing people’s wounds
HEALTH; Healing Treatment, 4,000 Years Old, Is Revived
Cut yourself? Tribal remedy of sprinkling SUGAR on wound heals it faster
Using Sugar To Treat Those Nasty Wounds
HONEY & SUGAR OUTPERFORM ANTIBIOTIC OINTMENTS IN TREATING WOUNDS AND BURNS
Posted in General.
rev="post-8868" 2 comments
– March 27, 2013
Trials and Errors: Why Science Is Failing Us
Also see:
Ben Goldacre: Battling bad science
- By Jonah Lehrer Email Author
- December 16, 2011 |
- Source
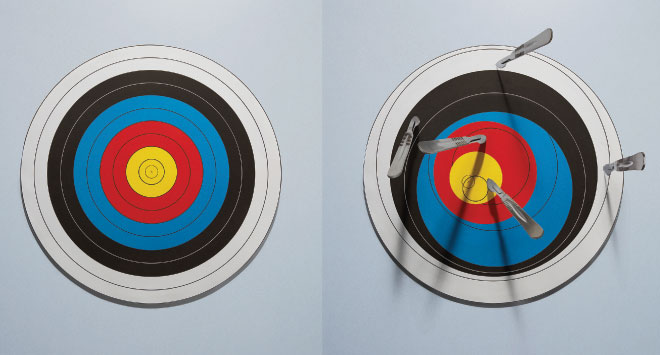
Photo: Mauricio Alejo
Every year, nearly $100 billion is invested in biomedical research in the US, all of it aimed at teasing apart the invisible bits of the body.
On November 30, 2006, executives at Pfizer—the largest pharmaceutical company in the world—held a meeting with investors at the firm’s research center in Groton, Connecticut. Jeff Kindler, then CEO of Pfizer, began the presentation with an upbeat assessment of the company’s efforts to bring new drugs to market. He cited “exciting approaches” to the treatment of Alzheimer’s disease, fibromyalgia, and arthritis. But that news was just a warm-up. Kindler was most excited about a new drug called torcetrapib, which had recently entered Phase III clinical trials, the last step before filing for FDA approval. He confidently declared that torcetrapib would be “one of the most important compounds of our generation.”
Kindler’s enthusiasm was understandable: The potential market for the drug was enormous. Like Pfizer’s blockbuster medication, Lipitor—the most widely prescribed branded pharmaceutical in America—torcetrapib was designed to tweak the cholesterol pathway. Although cholesterol is an essential component of cellular membranes, high levels of the compound have been consistently associated with heart disease. The accumulation of the pale yellow substance in arterial walls leads to inflammation. Clusters of white blood cells then gather around these “plaques,” which leads to even more inflammation. The end result is a blood vessel clogged with clumps of fat.
Lipitor works by inhibiting an enzyme that plays a key role in the production of cholesterol in the liver. In particular, the drug lowers the level of low-density lipoprotein (LDL), or so-called bad cholesterol. In recent years, however, scientists have begun to focus on a separate part of the cholesterol pathway, the one that produces high-density lipoproteins. One function of HDL is to transport excess LDL back to the liver, where it is broken down. In essence, HDL is a janitor of fat, cleaning up the greasy mess of the modern diet, which is why it’s often referred to as “good cholesterol.”
And this returns us to torcetrapib. It was designed to block a protein that converts HDL cholesterol into its more sinister sibling, LDL. In theory, this would cure our cholesterol problems, creating a surplus of the good stuff and a shortage of the bad. In his presentation, Kindler noted that torcetrapib had the potential to “redefine cardiovascular treatment.”
There was a vast amount of research behind Kindler’s bold proclamations. The cholesterol pathway is one of the best-understood biological feedback systems in the human body. Since 1913, when Russian pathologist Nikolai Anichkov first experimentally linked cholesterol to the buildup of plaque in arteries, scientists have mapped out the metabolism and transport of these compounds in exquisite detail. They’ve documented the interactions of nearly every molecule, the way hydroxymethylglutaryl-coenzyme A reductase catalyzes the production of mevalonate, which gets phosphorylated and condensed before undergoing a sequence of electron shifts until it becomes lanosterol and then, after another 19 chemical reactions, finally morphs into cholesterol. Furthermore, torcetrapib had already undergone a small clinical trial, which showed that the drug could increase HDL and decrease LDL. Kindler told his investors that, by the second half of 2007, Pfizer would begin applying for approval from the FDA. The success of the drug seemed like a sure thing.
And then, just two days later, on December 2, 2006, Pfizer issued a stunning announcement: The torcetrapib Phase III clinical trial was being terminated. Although the compound was supposed to prevent heart disease, it was actually triggering higher rates of chest pain and heart failure and a 60 percent increase in overall mortality. The drug appeared to be killing people.
That week, Pfizer’s value plummeted by $21 billion.
The story of torcetrapib is a tale of mistaken causation. Pfizer was operating on the assumption that raising levels of HDL cholesterol and lowering LDL would lead to a predictable outcome: Improved cardiovascular health. Less arterial plaque. Cleaner pipes. But that didn’t happen.
Such failures occur all the time in the drug industry. (According to one recent analysis, more than 40 percent of drugs fail Phase III clinical trials.) And yet there is something particularly disturbing about the failure of torcetrapib. After all, a bet on this compound wasn’t supposed to be risky. For Pfizer, torcetrapib was the payoff for decades of research. Little wonder that the company was so confident about its clinical trials, which involved a total of 25,000 volunteers. Pfizer invested more than $1 billion in the development of the drug and $90 million to expand the factory that would manufacture the compound. Because scientists understood the individual steps of the cholesterol pathway at such a precise level, they assumed they also understood how it worked as a whole.
This assumption—that understanding a system’s constituent parts means we also understand the causes within the system—is not limited to the pharmaceutical industry or even to biology. It defines modern science. In general, we believe that the so-called problem of causation can be cured by more information, by our ceaseless accumulation of facts. Scientists refer to this process as reductionism. By breaking down a process, we can see how everything fits together; the complex mystery is distilled into a list of ingredients. And so the question of cholesterol—what is its relationship to heart disease?—becomes a predictable loop of proteins tweaking proteins, acronyms altering one another. Modern medicine is particularly reliant on this approach. Every year, nearly $100 billion is invested in biomedical research in the US, all of it aimed at teasing apart the invisible bits of the body. We assume that these new details will finally reveal the causes of illness, pinning our maladies on small molecules and errant snippets of DNA. Once we find the cause, of course, we can begin working on a cure.

Photo: Mauricio Alejo
The problem with this assumption, however, is that causes are a strange kind of knowledge. This was first pointed out by David Hume, the 18th-century Scottish philosopher. Hume realized that, although people talk about causes as if they are real facts—tangible things that can be discovered—they’re actually not at all factual. Instead, Hume said, every cause is just a slippery story, a catchy conjecture, a “lively conception produced by habit.” When an apple falls from a tree, the cause is obvious: gravity. Hume’s skeptical insight was that we don’t see gravity—we see only an object tugged toward the earth. We look at X and then at Y, and invent a story about what happened in between. We can measure facts, but a cause is not a fact—it’s a fiction that helps us make sense of facts.
The truth is, our stories about causation are shadowed by all sorts of mental shortcuts. Most of the time, these shortcuts work well enough. They allow us to hit fastballs, discover the law of gravity, and design wondrous technologies. However, when it comes to reasoning about complex systems—say, the human body—these shortcuts go from being slickly efficient to outright misleading.
Consider a set of classic experiments designed by Belgian psychologist Albert Michotte, first conducted in the 1940s. The research featured a series of short films about a blue ball and a red ball. In the first film, the red ball races across the screen, touches the blue ball, and then stops. The blue ball, meanwhile, begins moving in the same basic direction as the red ball. When Michotte asked people to describe the film, they automatically lapsed into the language of causation. The red ball hit the blue ball, which caused it to move.
This is known as the launching effect, and it’s a universal property of visual perception. Although there was nothing about causation in the two-second film—it was just a montage of animated images—people couldn’t help but tell a story about what had happened. They translated their perceptions into causal beliefs.
Michotte then began subtly manipulating the films, asking the subjects how the new footage changed their description of events. For instance, when he introduced a one-second pause between the movement of the balls, the impression of causality disappeared. The red ball no longer appeared to trigger the movement of the blue ball. Rather, the two balls were moving for inexplicable reasons.
Michotte would go on to conduct more than 100 of these studies. Sometimes he would have a small blue ball move in front of a big red ball. When he asked subjects what was going on, they insisted that the red ball was “chasing” the blue ball. However, if a big red ball was moving in front of a little blue ball, the opposite occurred: The blue ball was “following” the red ball.
There are two lessons to be learned from these experiments. The first is that our theories about a particular cause and effect are inherently perceptual, infected by all the sensory cheats of vision. (Michotte compared causal beliefs to color perception: We apprehend what we perceive as a cause as automatically as we identify that a ball is red.) While Hume was right that causes are never seen, only inferred, the blunt truth is that we can’t tell the difference. And so we look at moving balls and automatically see causes, a melodrama of taps and collisions, chasing and fleeing.
The second lesson is that causal explanations are oversimplifications. This is what makes them useful—they help us grasp the world at a glance. For instance, after watching the short films, people immediately settled on the most straightforward explanation for the ricocheting objects. Although this account felt true, the brain wasn’t seeking the literal truth—it just wanted a plausible story that didn’t contradict observation.
This mental approach to causality is often effective, which is why it’s so deeply embedded in the brain. However, those same shortcuts get us into serious trouble in the modern world when we use our perceptual habits to explain events that we can’t perceive or easily understand. Rather than accept the complexity of a situation—say, that snarl of causal interactions in the cholesterol pathway—we persist in pretending that we’re staring at a blue ball and a red ball bouncing off each other. There’s a fundamental mismatch between how the world works and how we think about the world.
The good news is that, in the centuries since Hume, scientists have mostly managed to work around this mismatch as they’ve continued to discover new cause-and-effect relationships at a blistering pace. This success is largely a tribute to the power of statistical correlation, which has allowed researchers to pirouette around the problem of causation. Though scientists constantly remind themselves that mere correlation is not causation, if a correlation is clear and consistent, then they typically assume a cause has been found—that there really is some invisible association between the measurements.
Researchers have developed an impressive system for testing these correlations. For the most part, they rely on an abstract measure known as statistical significance, invented by English mathematician Ronald Fisher in the 1920s. This test defines a “significant” result as any data point that would be produced by chance less than 5 percent of the time. While a significant result is no guarantee of truth, it’s widely seen as an important indicator of good data, a clue that the correlation is not a coincidence.
 Photo: Mauricio Alejo
Photo: Mauricio Alejo
But here’s the bad news: The reliance on correlations has entered an age of diminishing returns. At least two major factors contribute to this trend. First, all of the easy causes have been found, which means that scientists are now forced to search for ever-subtler correlations, mining that mountain of facts for the tiniest of associations. Is that a new cause? Or just a statistical mistake? The line is getting finer; science is getting harder. Second—and this is the biggy—searching for correlations is a terrible way of dealing with the primary subject of much modern research: those complex networks at the center of life. While correlations help us track the relationship between independent measurements, such as the link between smoking and cancer, they are much less effective at making sense of systems in which the variables cannot be isolated. Such situations require that we understand every interaction before we can reliably understand any of them. Given the byzantine nature of biology, this can often be a daunting hurdle, requiring that researchers map not only the complete cholesterol pathway but also the ways in which it is plugged into other pathways. (The neglect of these secondary and even tertiary interactions begins to explain the failure of torcetrapib, which had unintended effects on blood pressure. It also helps explain the success of Lipitor, which seems to have a secondary effect of reducing inflammation.) Unfortunately, we often shrug off this dizzying intricacy, searching instead for the simplest of correlations. It’s the cognitive equivalent of bringing a knife to a gunfight.
These troubling trends play out most vividly in the drug industry. Although modern pharmaceuticals are supposed to represent the practical payoff of basic research, the R&D to discover a promising new compound now costs about 100 times more (in inflation-adjusted dollars) than it did in 1950. (It also takes nearly three times as long.) This trend shows no sign of letting up: Industry forecasts suggest that once failures are taken into account, the average cost per approved molecule will top $3.8 billion by 2015. What’s worse, even these “successful” compounds don’t seem to be worth the investment. According to one internal estimate, approximately 85 percent of new prescription drugs approved by European regulators provide little to no new benefit. We are witnessing Moore’s law in reverse.
This returns us to cholesterol, a compound whose scientific history reflects our tortured relationship with causes. At first, cholesterol was entirely bad; the correlations linked high levels of the substance with plaque. Years later, we realized that there were multiple kinds and that only LDL was bad. Then it became clear that HDL was more important than LDL, at least according to correlational studies and animal models. And now we don’t really know what matters, since raising HDL levels with torcetrapib doesn’t seem to help. Although we’ve mapped every known part of the chemical pathway, the causes that matter are still nowhere to be found. If this is progress, it’s a peculiar kind.
Back pain is an epidemic. The numbers are sobering: There’s an 80 percent chance that, at some point in your life, you’ll suffer from it. At any given time, about 10 percent of Americans are completely incapacitated by their lumbar regions, which is why back pain is the second most frequent reason people seek medical care, after general checkups. And all this treatment is expensive: According to a recent study in The Journal of the American Medical Association, Americans spend nearly $90 billion every year treating back pain, which is roughly equivalent to what we spend on cancer.
When doctors began encountering a surge in patients with lower back pain in the mid-20th century, as I reported for my 2009 book How We Decide, they had few explanations. The lower back is an exquisitely complicated area of the body, full of small bones, ligaments, spinal discs, and minor muscles. Then there’s the spinal cord itself, a thick cable of nerves that can be easily disturbed. There are so many moving parts in the back that doctors had difficulty figuring out what, exactly, was causing a person’s pain. As a result, patients were typically sent home with a prescription for bed rest.
This treatment plan, though simple, was still extremely effective. Even when nothing was done to the lower back, about 90 percent of people with back pain got better within six weeks. The body healed itself, the inflammation subsided, the nerve relaxed.
Over the next few decades, this hands-off approach to back pain remained the standard medical treatment. That all changed, however, with the introduction of magnetic resonance imaging in the late 1970s. These diagnostic machines use powerful magnets to generate stunningly detailed images of the body’s interior. Within a few years, the MRI machine became a crucial diagnostic tool.
The view afforded by MRI led to a new causal story: Back pain was the result of abnormalities in the spinal discs, those supple buffers between the vertebrae. The MRIs certainly supplied bleak evidence: Back pain was strongly correlated with seriously degenerated discs, which were in turn thought to cause inflammation of the local nerves. Consequently, doctors began administering epidurals to quiet the pain, and if it persisted they would surgically remove the damaged disc tissue.
But the vivid images were misleading. It turns out that disc abnormalities are typically not the cause of chronic back pain. The presence of such abnormalities is just as likely to be correlated with the absence of back problems, as a 1994 study published in The New England Journal of Medicine showed. The researchers imaged the spinal regions of 98 people with no back pain. The results were shocking: Two-thirds of normal patients exhibited “serious problems” like bulging or protruding tissue. In 38 percent of these patients, the MRI revealed multiple damaged discs. Nevertheless, none of these people were in pain. The study concluded that, in most cases, “the discovery of a bulge or protrusion on an MRI scan in a patient with low back pain may frequently be coincidental.”
Similar patterns appear in a new study by James Andrews, a sports medicine orthopedist. He scanned the shoulders of 31 professional baseball pitchers. Their MRIs showed that 90 percent of them had abnormal cartilage, a sign of damage that would typically lead to surgery. Yet they were all in perfect health.
This is not the way things are supposed to work. We assume that more information will make it easier to find the cause, that seeing the soft tissue of the back will reveal the source of the pain, or at least some useful correlations. Unfortunately, that often doesn’t happen. Our habits of visual conclusion-jumping take over. All those extra details end up confusing us; the more we know, the less we seem to understand.
The only solution for this mental flaw is to deliberately ignore a wealth of facts, even when the facts seem relevant. This is what’s happening with the treatment of back pain: Doctors are now encouraged to not order MRIs when making diagnoses. The latest clinical guidelines issued by the American College of Physicians and the American Pain Society strongly recommended that doctors “not routinely obtain imaging or other diagnostic tests in patients with nonspecific low back pain.”
And it’s not just MRIs that appear to be counterproductive. Earlier this year, John Ioannidis, a professor of medicine at Stanford, conducted an in-depth review of biomarkers in the scientific literature. Biomarkers are molecules whose presence, once detected, are used to infer illness and measure the effect of treatment. They have become a defining feature of modern medicine. (If you’ve ever had your blood drawn for lab tests, you’ve undergone a biomarker check. Cholesterol is a classic biomarker.) Needless to say, these tests depend entirely on our ability to perceive causation via correlation, to link the fluctuations of a substance to the health of the patient.
In his resulting paper, published in JAMA, Ioannidis looked at only the most highly cited biomarkers, restricting his search to those with more than 400 citations in the highest impact journals. He identified biomarkers associated with cardiovascular problems, infectious diseases, and the genetic risk of cancer. Although these causal stories had initially triggered a flurry of interest—several of the biomarkers had already been turned into popular medical tests—Ioannidis found that the claims often fell apart over time. In fact, 83 percent of supposed correlations became significantly weaker in subsequent studies.
Consider the story of homocysteine, an amino acid that for several decades appeared to be linked to heart disease. The original paper detecting this association has been cited 1,800 times and has led doctors to prescribe various B vitamins to reduce homocysteine. However, a study published in 2010—involving 12,064 volunteers over seven years—showed that the treatment had no effect on the risk of heart attack or stroke, despite the fact that homocysteine levels were lowered by nearly 30 percent.
The larger point is that we’ve constructed our $2.5 trillion health care system around the belief that we can find the underlying causes of illness, the invisible triggers of pain and disease. That’s why we herald the arrival of new biomarkers and get so excited by the latest imaging technologies. If only we knew more and could see further, the causes of our problems would reveal themselves. But what if they don’t?
The failure of this drug in particular has not ended the development of new cholesterol medications. The potential market for them is simply too huge.
The failure of torcetrapib has not ended the development of new cholesterol medications—the potential market is simply too huge. Although the compound is a sobering reminder that our causal beliefs are defined by their oversimplifications, that even the best-understood systems are still full of surprises, scientists continue to search for the magic pill that will make cardiovascular disease disappear. Ironically, the latest hyped treatment, a drug developed by Merck called anacetrapib, inhibits the exact same protein as torcetrapib. The initial results of the clinical trial, which were made public in November 2010, look promising. Unlike its chemical cousin, this compound doesn’t appear to raise systolic blood pressure or cause heart attacks. (A much larger clinical trial is under way to see whether the drug saves lives.) Nobody can conclusively explain why these two closely related compounds trigger such different outcomes or why, according to a 2010 analysis, high HDL levels might actually be dangerous for some people. We know so much about the cholesterol pathway, but we never seem to know what matters.
Chronic back pain also remains a mystery. While doctors have long assumed that there’s a valid correlation between pain and physical artifacts—a herniated disc, a sheared muscle, a pinched nerve—there’s a growing body of evidence suggesting the role of seemingly unrelated factors. For instance, a recent study published in the journal Spine concluded that minor physical trauma had virtually no relationship with disabling pain. Instead, the researchers found that a small subset of “nonspinal factors,” such as depression and smoking, were most closely associated with episodes of serious pain. We keep trying to fix the back, but perhaps the back isn’t what needs fixing. Perhaps we’re searching for causes in the wrong place.
The same confusion afflicts so many of our most advanced causal stories. Hormone replacement therapy was supposed to reduce the risk of heart attack in postmenopausal women—estrogen prevents inflammation in blood vessels—but a series of recent clinical trials found that it did the opposite, at least among older women. (Estrogen therapy was also supposed to ward off Alzheimer’s, but that doesn’t seem to work, either.) We were told that vitamin D supplements prevented bone loss in people with multiple sclerosis and that vitamin E supplements reduced cardiovascular disease—neither turns out to be true.
It would be easy to dismiss these studies as the inevitable push and pull of scientific progress; some papers are bound to get contradicted. What’s remarkable, however, is just how common such papers are. One study, for instance, analyzed 432 different claims of genetic links for various health risks that vary between men and women. Only one of these claims proved to be consistently replicable. Another meta review, meanwhile, looked at the 49 most-cited clinical research studies published between 1990 and 2003. Most of these were the culmination of years of careful work. Nevertheless, more than 40 percent of them were later shown to be either totally wrong or significantly incorrect. The details always change, but the story remains the same: We think we understand how something works, how all those shards of fact fit together. But we don’t.
Given the increasing difficulty of identifying and treating the causes of illness, it’s not surprising that some companies have responded by abandoning entire fields of research. Most recently, two leading drug firms, AstraZeneca and GlaxoSmithKline, announced that they were scaling back research into the brain. The organ is simply too complicated, too full of networks we don’t comprehend.
David Hume referred to causality as “the cement of the universe.” He was being ironic, since he knew that this so-called cement was a hallucination, a tale we tell ourselves to make sense of events and observations. No matter how precisely we knew a given system, Hume realized, its underlying causes would always remain mysterious, shadowed by error bars and uncertainty. Although the scientific process tries to makes sense of problems by isolating every variable—imagining a blood vessel, say, if HDL alone were raised—reality doesn’t work like that. Instead, we live in a world in which everything is knotted together, an impregnable tangle of causes and effects. Even when a system is dissected into its basic parts, those parts are still influenced by a whirligig of forces we can’t understand or haven’t considered or don’t think matter. Hamlet was right: There really are more things in heaven and Earth than are dreamt of in our philosophy.
This doesn’t mean that nothing can be known or that every causal story is equally problematic. Some explanations clearly work better than others, which is why, thanks largely to improvements in public health, the average lifespan in the developed world continues to increase. (According to the Centers for Disease Control and Prevention, things like clean water and improved sanitation—and not necessarily advances in medical technology—accounted for at least 25 of the more than 30 years added to the lifespan of Americans during the 20th century.) Although our reliance on statistical correlations has strict constraints—which limit modern research—those correlations have still managed to identify many essential risk factors, such as smoking and bad diets.
And yet, we must never forget that our causal beliefs are defined by their limitations. For too long, we’ve pretended that the old problem of causality can be cured by our shiny new knowledge. If only we devote more resources to research or dissect the system at a more fundamental level or search for ever more subtle correlations, we can discover how it all works. But a cause is not a fact, and it never will be; the things we can see will always be bracketed by what we cannot. And this is why, even when we know everything about everything, we’ll still be telling stories about why it happened. It’s mystery all the way down.
Posted in General.
rev="post-8854" 1 comment
– March 24, 2013
Bert Hill Coaches Charlie Francis Speed Rx to the Detroit Lions
Posted in General.
Comments Off on Bert Hill Coaches Charlie Francis Speed Rx to the Detroit Lions
– March 22, 2013
Estrogen and Bowel Transit Time
Also see:
Ray Peat, PhD on the Benefits of the Raw Carrot
Dietary Fiber, Bowel Health, and Cancer
Hormonal profiles in women with breast cancer
Endometriosis and Estrogen
The effect of raw carrot on serum lipids and colon function
Protective Bamboo Shoots
Endotoxin-lipoprotein Hypothesis
Endotoxin: Poisoning from the Inside Out
Protection from Endotoxin
Bowel Toxins Accelerate Aging
Protective Cascara Sagrada and Emodin
Fermentable Carbohydrates, Anxiety, Aggression
Intestinal Serotonin and Bone Loss
Autoimmunity and Intestinal Flora
“Undigestible fiber, if it isn’t broken down by bowel bacteria, increases fecal bulk, and tends to speed the transit of material through the intestine, just as laxatives do. But some of these “fiber” materials, e.g., lignin, are themselves estrogenic, and other fibers, by promoting bacterial growth, can promote the conversion of harmless substances into toxins and carcinogens. When there is a clear “antiestrogen” effect from dietary fiber, it seems to be the result of accelerated transit through the intestine, speeding elimination and preventing reabsorption of the estrogen which has been excreted in the bile. Laxatives have this same effect on the excretion of estradiol.” -Ray Peat, PhD
Accelerated bowel transit time reduced estrogen:
Br J Cancer. 1997;76(3):395-400.
Lower serum oestrogen concentrations associated with faster intestinal transit.
Lewis SJ, Heaton KW, Oakey RE, McGarrigle HH.
Increased fibre intake has been shown to reduce serum oestrogen concentrations. We hypothesized that fibre exerts this effect by decreasing the time available for reabsorption of oestrogens in the colon. We tested this in volunteers by measuring changes in serum oestrogen levels in response to manipulation of intestinal transit times with senna and loperamide, then comparing the results with changes caused by wheat bran. Forty healthy premenopausal volunteers were placed at random into one of three groups. The first group took senna for two menstrual cycles then, after a washout period, took wheat bran, again for two menstrual cycles. The second group did the reverse. The third group took loperamide for two menstrual cycles. At the beginning and end of each intervention a 4-day dietary record was kept and whole-gut transit time was measured; stools were taken for measurement of pH and beta-glucuronidase activity and blood for measurement of oestrone and oestradiol and their non-protein-bound fractions and of oestrone sulphate. Senna and loperamide caused the intended alterations in intestinal transit, whereas on wheat bran supplements there was a trend towards faster transit. Serum oestrone sulphate fell with wheat bran (mean intake 19.8 g day(-1)) and with senna; total- and non-protein-bound oestrone fell with senna. No significant changes in serum oestrogens were seen with loperamide. No significant changes were seen in faecal beta-glucuronidase activity. Stool pH changed only with senna, in which case it fell. In conclusion, speeding up intestinal transit can lower serum oestrogen concentrations.
Eur J Gastroenterol Hepatol. 1998 Jan;10(1):33-9.
Intestinal absorption of oestrogen: the effect of altering transit-time.
Lewis SJ, Oakey RE, Heaton KW.
OBJECTIVE:
The mechanism by which a high fibre diet may reduce serum oestrogens is unknown. We hypothesized that time is a rate-limiting factor in oestrogen absorption from the colon so that changes in colonic transit-rate affect the proportion of oestrogen that is deconjugated and/or absorbed.
AIM:
To determine if alteration of intestinal transit rate would influence the absorption of an oral dose of oestradiol glucuronide.
PARTICIPANTS:
Twenty healthy postmenopausal women recruited by advertisement.
SETTING:
Department of Medicine, Bristol Royal Infirmary.
METHODS:
Volunteers consumed, in turn, wheat bran, senna, loperamide and bran shaped plastic flakes, each for 10 days with a minimum 2 week washout period between study periods, dietary intake being unchanged. Before and in the last 4 days of each intervention whole-gut transit-time, defecation frequency, stool form, stool beta-glucuronidase activity, stool pH and the absorption of a 1.5 mg dose of oestradiol glucuronide were measured.
RESULTS:
Wheat bran, senna and plastic flakes led to the intended reduction in whole-gut transit-time, increase in defecatory frequency and increase in stool form score. Loperamide caused the opposite effect. The length of time the absorbed oestrogen was detectable in the serum fell with wheat bran and senna, although this was only significant for oestradiol. Oestrone, but not oestradiol, was detectable for a longer time with loperamide. Plastic flakes had no effect on either oestrogen. Areas under the curve did not change significantly but tended to fall with the three transit-accelerating agents and to rise with loperamide.
CONCLUSION:
Our data indicate there is likely to be an effect of intestinal transit on the absorption of oestrogens but more refined techniques are needed to characterize this properly.
Estrogen slows bowel transit time:
Res Nurs Health. 1998 Jun;21(3):221-8.
Estrogen suppresses gastric motility response to thyrotropin-releasing hormone and stress in awake rats.
Bond EF, Heitkemper MM, Bailey SL.
Symptoms associated with gastric motility alteration vary with stress and ovarian hormone status, most notably in women with irritable bowel syndrome. This study examines combined effects, comparing gastric motility during administration of a stress-related neuropeptide thyrotropin-releasing hormone (TRH) and restraint stress in conscious rats of varied ovarian hormone status. Adult rats were ovariectomized and implanted with estrogen, progesterone, or vehicle-releasing pellets. After 21 days, intracerebroventricular (i.c.) cannula and gastric tension transducer were implanted. After 25-27 days, motility was recorded during neuropeptide injection (TRH/saline i.c.) or restraint stress. TRH induced increased motility in all groups; the response varied with hormone group, and was least and briefest in estrogen-treated rats. Motility during restraint varied with hormone group; it was diminished in estrogen-treated but not other groups. Ovarian hormone status (estrogen) modifies gut response to TRH and restraint stress.
Intestinal flora, diet, and estrogen:
Rev Infect Dis. 1984 Mar-Apr;6 Suppl 1:S85-90.
Estrogens, breast cancer, and intestinal flora.
Gorbach SL.
Epidemiologic evidence has linked diet to breast cancer, with the highest cancer rates observed in women who eat a high fat-low fiber diet. There is also substantial information, both clinical and experimental, that implicates estrogens in the etiology of breast cancer. A recent study from our laboratory has shown that diet influences levels of estrogens, and the main mechanism is metabolism of estrogens in the intestine. The intestinal microflora plays a key role in the enterohepatic circulation of estrogens by deconjugating bound estrogens that appear in the bile, thereby permitting the free hormones to be reabsorbed. By suppressing the microflora with antibiotic therapy, fecal estrogens increase and urinary estrogens decrease, changes indicating diminished intestinal reabsorption. A low fat-high fiber diet is associated with similar findings-high fecal estrogens and low urinary estrogens. It appears that the microflora plays a key role in the metabolism of female sex hormones.
Posted in General.
Comments Off on Estrogen and Bowel Transit Time
– March 22, 2013
Serotonin and Autism Connection
Also see:
Antidepressant use in pregnancy linked to autism risk in boys: Study
Hypothyroidism and Serotonin
Estrogen Increases Serotonin
Tryptophan Metabolism: Effects of Progesterone, Estrogen, and PUFA
Omega -3 “Deficiency” Decreases Serotonin Producing Enzyme
Serotonin Reuptake ENHANCER as Anti-Depressant
Therapeutic Effects of Bromocriptine
Acute Appendicitis and Serotonin
Enzyme to Know: Tryptophan Hydroxylase
Serotonin and Melatonin Lower Progesterone
Role of Serotonin in Preeclampsia
PUFA, Development, and Allergy Incidence
Maternal exposure to anti-depressant SSRIs linked to autism in children
“In autism, repetitive motions are a common symptom, and serotonin is high in the blood serum and platelets of autistic children and their relatives.” -Ray Peat, PhD
Med Hypotheses. 2010 May;74(5):880-3. doi: 10.1016/j.mehy.2009.11.015. Epub 2009 Dec 16.
Serotonin, pregnancy and increased autism prevalence: is there a link?
Hadjikhani N.
The prevalence of autism, a neurodevelopmental condition resulting from genetic and environmental causes, has increased dramatically during the last decade. Among the potential environmental factors, hyperserotonemia during pregnancy and its effect on brain development could be playing a role in this prevalence raise. In the rodent model developed by Whitaker-Azmitia and colleagues, hyperserotonemia during fetal development results in a dysfunction of the hypothalamo-pituitary axis, affecting the amygdala as well as pro-social hormone oxytocin regulation. Dysfunction of the amygdala and abnormal oxytocin levels may underlie many clinical features of ASD. Selective serotonin reuptake inhibitors (SSRI) are the most widely used class of antidepressants drugs, and they are not contraindicated during pregnancy. In this paper, we hypothesize that increased serotonemia during pregnancy, including due to SSRI intake, could be one of the causes of the raising prevalence in autism. If our hypothesis is confirmed, it will not only shed light on one of the possible reason for autism prevalence, but also offer new preventive and treatment options.
J Neuropsychiatry Clin Neurosci. 1990 Summer;2(3):268-74.
Autistic children and their first-degree relatives: relationships between serotonin and norepinephrine levels and intelligence.
Cook EH Jr, Leventhal BL, Heller W, Metz J, Wainwright M, Freedman DX.
Whole-blood serotonin (5-HT) and plasma norepinephrine (NE) were studied in 16 autistic children, 21 siblings of autistic children, and 53 parents of autistic children. Both plasma NE and whole-blood 5-HT were negatively correlated with vocabulary performance. Whole-blood 5-HT and plasma NE did not differ between autistic children with or without histories of self-injurious behavior or decreased pain sensitivity. Eighteen subjects were hyperserotonemic (whole-blood 5-HT greater than 270 ng/ml). For these subjects, plasma NE was significantly higher than for subjects without hyperserotonemia. Seven of 10 families with one hyperserotonemic member had two or more hyperserotonemic members. Observations of familiarity of whole-blood 5-HT suggest that larger-scale and more focused study of whole-blood 5-HT as a possible genetic marker may be productive.
J Autism Dev Disord. 1990 Dec;20(4):499-511.
Relationships of whole blood serotonin and plasma norepinephrine within families.
Leventhal BL, Cook EH Jr, Morford M, Ravitz A, Freedman DX.
Whole blood serotonin (5HT) and plasma norepinephrine (NE) levels were determined in 47 families of autistic probands to study relationships within families of these measures. Whole blood 5HT, but not plasma NE, was significantly positively correlated between autistic children and their mothers, fathers, and siblings. Twenty-three of the 47 families studied had at least 1 hyperserotonemic member. Of these 23 families, 10 (43.5%) had 2 or more hyperserotonemic members; 5 families were identified in which each family member studied had hyperserotonemia (whole blood 5HT greater than 270 ng/ml). If the autistic child of a family was hyperserotonemic, the first-degree relatives were 2.4 times more likely to be hypersertonemic than if the autistic child was not hyperserotonemic. Mean whole blood 5HT levels were higher in autistic subjects than their parents or siblings. Siblings were found to have lower plasma NE than autistic probands. This study replicates a previous study showing familial relationships of hyperserotonemia within families with autistic children.
Arch Gen Psychiatry. 1977 May;34(5):521-31.
Hyperserotonemia and amine metabolites in autistic and retarded children.
Hanley HG, Stahl SM, Freedman DX.
Mean whole blood serotonin (5-HT) levels were elevated in groups of autistic and severely retarded children. Eight of 27 (30%) individual autistic children, 13 of 25 (52%) severely retarded children, two of 23 (9%) mildly retarded children, and none of the control children had statistically significant blood 5-HT levels elevations (hyperserotonemia). Hyperserotonemic autistic children excreted more urinary 5-HT, 5-hydroxyindoleacetic acid (5-HIAA), tryptamine, and vanillylmandelic acid than did mildly retarded children with normal blood 5-HT levels. Rates of depletion and repletion of blood 5-HT levels in these two groups following reserpine therapy were identical. Oral tryptophan administration doubled urinary 5-HIAA excretion in both groups and raised urinary 5-HT levels in hyperserotonemic autistic children, but lowered urinary 5-HT in mildly retarded, normal blood 5-HT children. No clear mechanism for hyperserotonemia was found; the rationale for further investigations is discussed.
Int J Dev Neurosci. 2005 Feb;23(1):75-83.
Behavioral and cellular consequences of increasing serotonergic activity during brain development: a role in autism?
Whitaker-Azmitia PM.
The hypothesis explored in this review is that the high levels of serotonin in the blood seen in some autistic children (the so-called hyperserotonemia of autism) may lead to some of the behavioral and cellular changes also observed in the disorder. At early stages of development, when the blood-brain Barrier is not yet fully formed, the high levels of serotonin in the blood can enter the brain of a developing fetus and cause loss of serotonin terminals through a known negative feedback function of serotonin during development. The loss of serotonin innervation persists throughout subsequent development and the symptoms of autism appear. A review of the basic scientific literature on prenatal treatments affecting serotonin is given, in support of this hypothesis, with an emphasis on studies using the serotonin agonist, 5-methoxytryptamine (5-MT). In work using 5-MT to mimic hyperserotonemia, Sprague-Dawley rats are treated from gestational day 12 until postnatal 20. In published reports, these animals have been found to have a significant loss of serotonin terminals, decreased metabolic activity in cortex, changes in columnar development in cortex, changes in serotonin receptors, and “autistic-like” behaviors. In preliminary cellular findings given in this review, the animals have also been found to have cellular changes in two relevant brain regions: 1. Central nucleus of the amygdala, a brain region involved in fear-responding, where an increase in calcitonin gene related peptide (CGRP) was found 2. Paraventricular nucleus of the hypothalamus, a brain region involved in social memory and bonding, where a decrease in oxytocin was found. Both of these cellular changes could result from loss of serotonin innervation, possibly due to loss of terminal outgrowth from the same cells of the raphe nuclei. Thus, increased serotonergic activity during development could damage neurocircuitry involved in emotional responding to social stressors and may have relevance to the symptoms of autism.
Physiol Behav. 2002 Mar;75(3):403-10.
Behavioral and magnetic resonance spectroscopic studies in the rat hyperserotonemic model of autism.
Kahne D, Tudorica A, Borella A, Shapiro L, Johnstone F, Huang W, Whitaker-Azmitia PM.
Autism is classified as a pervasive developmental disorder, with several cardinal features including sensory disturbances, obsessive-compulsive-like behavior, lack of bonding to caregivers and motor disturbances. To date, there is a lack of an animal model of the disease. The current work is aimed at producing such a model by treating developing rat pups with a serotonergic agonist, 5-methoxytryptamine (5-MT; 1 mg/kg) during development (from gestational age 12 days to postnatal day 20), thus mimicking one of the hallmark neurochemical features of the illness-increases in the neurotransmitter, serotonin. Animals were then tested in behavioral paradigms that may resemble the human illness. Treated rat pups were found to be overreactive to auditory or tactile sensory stimuli, to display changes in the negative geotaxic test of motor development, to show lack of separation-induced vocalizations when their dam was removed and to show decreased alternation in the spontaneous alternation task. As well, the animals showed metabolic abnormalities in the brain using in vivo proton magnetic resonance spectroscopy, which are consistent with those observed in autistic children. In summary, the model we are proposing shows some of the behavioral and metabolic features of autism, as well as being produced through alteration of a neurochemical system known to be altered in autism.
The Journal of Neuroscience, 1 June 2016, 36(22): 6041-6049; doi: 10.1523/JNEUROSCI.2534-15.2016
Maternal Inflammation Disrupts Fetal Neurodevelopment via Increased Placental Output of Serotonin to the Fetal Brain
Nick Goeden1, Juan Velasquez, Kathryn A. Arnold, Yen Chan, Brett T. Lund, George M. Anderson6, and Alexandre Bonnin
Maternal inflammation during pregnancy affects placental function and is associated with increased risk of neurodevelopmental disorders in the offspring. The molecular mechanisms linking placental dysfunction to abnormal fetal neurodevelopment remain unclear. During typical development, serotonin (5-HT) synthesized in the placenta from maternal L-tryptophan (TRP) reaches the fetal brain. There, 5-HT modulates critical neurodevelopmental processes. We investigated the effects of maternal inflammation triggered in midpregnancy in mice by the immunostimulant polyriboinosinic-polyribocytidylic acid [poly(I:C)] on TRP metabolism in the placenta and its impact on fetal neurodevelopment. We show that a moderate maternal immune challenge upregulates placental TRP conversion rapidly to 5-HT through successively transient increases in substrate availability and TRP hydroxylase (TPH) enzymatic activity, leading to accumulation of exogenous 5-HT and blunting of endogenous 5-HT axonal outgrowth specifically within the fetal forebrain. The pharmacological inhibition of TPH activity blocked these effects. These results establish altered placental TRP conversion to 5-HT as a new mechanism by which maternal inflammation disrupts 5-HT-dependent neurogenic processes during fetal neurodevelopment.
SIGNIFICANCE STATEMENT The mechanisms linking maternal inflammation during pregnancy with increased risk of neurodevelopmental disorders in the offspring are poorly understood. In this study, we show that maternal inflammation in midpregnancy results in an upregulation of tryptophan conversion to serotonin (5-HT) within the placenta. Remarkably, this leads to exposure of the fetal forebrain to increased concentrations of this biogenic amine and to specific alterations of crucially important 5-HT-dependent neurogenic processes. More specifically, we found altered serotonergic axon growth resulting from increased 5-HT in the fetal forebrain. The data provide a new understanding of placental function playing a key role in fetal brain development and how this process is altered by adverse prenatal events such as maternal inflammation. The results uncover important future directions for understanding the early developmental origins of mental disorders.
Posted in General.
Comments Off on Serotonin and Autism Connection
– March 21, 2013
Alice Stewart: The woman who knew too much
Also see:
Alice Mary Stewart
Alice Stewart, 95; Linked X-Rays to Diseases
Dr. Alice Stewart, Low-Level Radiation, and the Fetus
Book: The Woman Who Knew Too Much: Alice Stewart and the Secrets of Radiation
Inflammation from Radiation
Harm of Prenatal Exposure to Radiation
Caffeine and Skin Protection
Topical Vitamin E and ultraviolet radiation on human skin
Radiation and Growth – Ray Peat
Bone Density: First Do No Harm
Executive Summary, Radiation from Medical Procedures in the Pathogenesis of Cancer and Ischemic Heart Disease: Dose-Response Studies with Physicians per 100,000 Population
Quotes and more from Dr. John Gofman
John W. Gofman, 88, Scientist and Advocate for Nuclear Safety, Dies
Breast Cancer
Alice Stewart was one of Britain’s foremost epidemiologists. However her recognition came late in her career, having spent her life fighting the establishment’s enshrined views.
In the 1950s when she started her work, x-rays were routinely used in foetal monitoring. It was Stewart who first showed the link between the practice and childhood leukemia. She went on to look at the effects of low-level radiation exposure – uncovering the true adverse effects of chronic exposure, and thus earning herself the enmity of the nuclear industry.
Posted in General.
Comments Off on Alice Stewart: The woman who knew too much
– March 19, 2013
Vitamin K, Calcification, & Atherosclerosis
Also See:
Intestinal Bacteria Synthesize Vitamin K2
Bone Health and Vitamin K
Calcium to Phosphorus Ratio, PTH, and Bone Health
Intestinal Serotonin and Bone Loss
Carbohydrates and Bone Health
Parmigiano Reggiano cheese and bone health
Calcium Paradox
Blood Pressure Management with Calcium & Dairy
Hypertension and Calcium Deficiency
Excess Dietary Phosphorus Lowers Vitamin D Levels
Fatty Acid Synthase (FAS), Vitamin D, and Cancer
ARTERIOSCLEROSIS CAN BE REVERSED by Dr. James Howenstine, MD
Food Nutr Res. 2012;56. doi: 10.3402/fnr.v56i0.5329. Epub 2012 Apr 2.
Vitamin K: the effect on health beyond coagulation – an overview.
Vermeer C.
Vitamin K is essential for the synthesis of proteins belonging to the Gla-protein family. To the members of this family belong four blood coagulation factors, which all are exclusively formed in the liver. The importance of vitamin K for hemostasis is demonstrated from the fact that vitamin K-deficiency is an acute, life-threatening condition due to excessive bleeding. Other members of the Gla-protein family are osteocalcin, matrix Gla-protein (MGP), and Gas6 that play key functions in maintaining bone strength, arterial calcification inhibition, and cell growth regulation, respectively. In total 17 Gla-proteins have been discovered at this time. Recently, it was observed that the dietary vitamin K requirement for the synthesis of the coagulation factors is much lower than for that of the extra-hepatic Gla-proteins. This forms the basis of the triage theory stating that during poor dietary supply, vitamins are preferentially utilized for functions that are important for immediate survival. This explains why in the healthy population all clotting factors are synthesized in their active form, whereas the synthesis of other Gla-proteins is sub-optimal in non-supplemented subjects. Prolonged sub-clinical vitamin K deficiency is a risk factor for osteoporosis, atherosclerosis, and cancer. Present recommendations for dietary intake are based on the daily dose required to prevent bleeding. Accumulating scientific data suggests that new, higher recommendations for vitamin K intake should be formulated.
Menopause Int. 2011 Mar;17(1):19-23. doi: 10.1258/mi.2011.011006.
Vitamin K, osteoporosis and degenerative diseases of ageing.
Vermeer C, Theuwissen E.
The function of vitamin K is to serve as a co-factor during the post-translational carboxylation of glutamate (Glu) residues into γ-carboxyglutamate (Gla) residues. The vital importance of the Gla-proteins essential for normal haemostasis is well recognized. During recent years, new Gla-containing proteins have been discovered and the vitamin K-dependent carboxylation is also essential for their function. It seems, however, that our dietary vitamin K intake is too low to support the carboxylation of at least some of these Gla-proteins. According to the triage theory, long-term vitamin K inadequacy is an independent, but modifiable risk factor for the development of degenerative diseases of ageing including osteoporosis and atherosclerosis
Eur J Nutr. 2004 Dec;43(6):325-35. Epub 2004 Feb 5.
Beyond deficiency: potential benefits of increased intakes of vitamin K for bone and vascular health.
Vermeer C, Shearer MJ, Zittermann A, Bolton-Smith C, Szulc P, Hodges S, Walter P, Rambeck W, Stöcklin E, Weber P.
Vitamin K is well known for its role in the synthesis of a number of blood coagulation factors. During recent years vitamin K-dependent proteins were discovered to be of vital importance for bone and vascular health. Recommendations for dietary vitamin K intake have been made on the basis of the hepatic requirements for the synthesis of blood coagulation factors. Accumulating evidence suggests that the requirements for other functions than blood coagulation may be higher. This paper is the result of a closed workshop (Paris, November 2002) in which a number of European vitamin K experts reviewed the available data and formulated their standpoint with respect to recommended dietary vitamin K intake and the use of vitamin K-containing supplements.
PM R. 2011 Jun;3(6 Suppl 1):S82-7. doi: 10.1016/j.pmrj.2011.04.008.
Vitamin K: fracture prevention and beyond.
Falcone TD, Kim SS, Cortazzo MH.
Morbidity and decreased function related to osteoporosis, fracture, cardiovascular disease, stroke, and peripheral vascular disease are encountered by clinicians daily. Although we have seen vast advancement in treatment and management of these conditions, preventative practice has unfortunately served a lesser role in patient care. Increasing the dietary intake of vitamin K may have substantial utility in the prevention of these disease states. Since the discovery of vitamin K in 1935, its primary role was thought to be involved in the synthesis of clotting factors II, VII, IX, and X. Recently, its function in other metabolic pathways has emerged, leading to exploration of its significance beyond coagulation. Vitamin K is essential to bone physiology and prevention of atherosclerosis. It is involved in bone remodeling, cell signaling, apoptosis, arterial calcification, and chemotaxis, and it has anti-inflammatory effects. Conversely, warfarin, a potent vitamin K inhibitor, has demonstrated adverse effects on bone remodeling and atherosclerosis. Natural forms of vitamin K are available in multiple dietary sources, and some structural forms are more readily available for use in metabolic pathways than are others. With regard to supplementation, the specific form of vitamin K is often not disclosed, and the recommended daily value is potentially less than what is physiologically required. On the basis of a review of the literature, it appears advantageous to encourage patients to eat a diet rich in vitamin K; however, the benefit of vitamin K supplementation alone is yet to be thoroughly conveyed.
Atherosclerosis. 1995 Jul;116(1):117-23.
Vitamin K intake and osteocalcin levels in women with and without aortic atherosclerosis: a population-based study.
Jie KS, Bots ML, Vermeer C, Witteman JC, Grobbee DE.
Protein-bound gamma-carboxyglutamate (Gla) has been demonstrated in calcified atherosclerotic plaques. Vitamin K is required for the formation of Gla-residues. As the biological activity of Gla-proteins appears to be strictly dependent on the presence of the Gla-residues, vitamin K status may be an important factor in the development and progression of atherosclerotic calcifications. We studied the association of vitamin K status, as assessed by nutritional vitamin K intake and the measurements of two circulating immunoreactive osteocalcin (irOC) fractions, with aortic atherosclerosis in a population-based study of 113 postmenopausal women. Women with calcified lesions (n = 34) had a 42.9 micrograms lower mean age-adjusted dietary vitamin K intake/day (95% C.I. -6.6 to 92.5) than those without calcifications (n = 79). Atherosclerotic women had higher irOC levels with a low affinity for hydroxyapatite (irOCfree): age-adjusted difference of 0.32 ng/ml (95% C.I. 0.03 to 0.61). In addition, the high affinity irOC levels expressed as a percentage (hydroxyapatite binding capacity, HBC) were 5.12% (95% C.I. 1.32 to 8.92) lower in women with calcifications. Our study indicates that women with aortic atherosclerosis have an impaired vitamin K status as reflected by a lower nutritional vitamin K intake, an increased irOCfree level and a reduced HBC level. An impaired vitamin K status in subjects with atherosclerosis is compatible with the view that vitamin K or Gla-containing proteins are involved in the development of calcification of the vessel wall.
PLoS One. 2012;7(8):e43229. doi: 10.1371/journal.pone.0043229. Epub 2012 Aug 29.
Vitamin K-antagonists accelerate atherosclerotic calcification and induce a vulnerable plaque phenotype.
Schurgers LJ, Joosen IA, Laufer EM, Chatrou ML, Herfs M, Winkens MH, Westenfeld R, Veulemans V, Krueger T, Shanahan CM, Jahnen-Dechent W, Biessen E, Narula J, Vermeer C, Hofstra L, Reutelingsperger CP.
BACKGROUND:
Vitamin K-antagonists (VKA) are treatment of choice and standard care for patients with venous thrombosis and thromboembolic risk. In experimental animal models as well as humans, VKA have been shown to promote medial elastocalcinosis. As vascular calcification is considered an independent risk factor for plaque instability, we here investigated the effect of VKA on coronary calcification in patients and on calcification of atherosclerotic plaques in the ApoE(-/-) model of atherosclerosis.
METHODOLOGY/PRINCIPAL FINDINGS:
A total of 266 patients (133 VKA users and 133 gender and Framingham Risk Score matched non-VKA users) underwent 64-slice MDCT to assess the degree of coronary artery disease (CAD). VKA-users developed significantly more calcified coronary plaques as compared to non-VKA users. ApoE(-/-) mice (10 weeks) received a Western type diet (WTD) for 12 weeks, after which mice were fed a WTD supplemented with vitamin K(1) (VK(1), 1.5 mg/g) or vitamin K(1) and warfarin (VK(1)&W; 1.5 mg/g & 3.0 mg/g) for 1 or 4 weeks, after which mice were sacrificed. Warfarin significantly increased frequency and extent of vascular calcification. Also, plaque calcification comprised microcalcification of the intimal layer. Furthermore, warfarin treatment decreased plaque expression of calcification regulatory protein carboxylated matrix Gla-protein, increased apoptosis and, surprisingly outward plaque remodeling, without affecting overall plaque burden.
CONCLUSIONS/SIGNIFICANCE:
VKA use is associated with coronary artery plaque calcification in patients with suspected CAD and causes changes in plaque morphology with features of plaque vulnerability in ApoE(-/-) mice. Our findings underscore the need for alternative anticoagulants that do not interfere with the vitamin K cycle.
Adv Nutr. 2012 Mar 1;3(2):158-65. doi: 10.3945/an.111.001644.
Vitamin K status and vascular calcification: evidence from observational and clinical studies.
Shea MK, Holden RM.
Vascular calcification occurs when calcium accumulates in the intima (associated with atherosclerosis) and/or media layers of the vessel wall. Coronary artery calcification (CAC) reflects the calcium burden within the intima and media of the coronary arteries. In population-based studies, CAC independently predicts cardiovascular disease (CVD) and mortality. A preventive role for vitamin K in vascular calcification has been proposed based on its role in activating matrix Gla protein (MGP), a calcification inhibitor that is expressed in vascular tissue. Although animal and in vitro data support this role of vitamin K, overall data from human studies are inconsistent. The majority of population-based studies have relied on vitamin K intake to measure status. Phylloquinone is the primary dietary form of vitamin K and available supplementation trials, albeit limited, suggest phylloquinone supplementation is relevant to CAC. Yet observational studies have found higher dietary menaquinone, but not phylloquinone, to be associated with less calcification. Vascular calcification is highly prevalent in certain patient populations, especially in those with chronic kidney disease (CKD), and it is plausible vitamin K may contribute to reducing vascular calcification in patients at higher risk. Subclinical vitamin K deficiency has been reported in CKD patients, but studies linking vitamin K status to calcification outcomes in CKD are needed to clarify whether or not improving vitamin K status is associated with improved vascular health in CKD. This review summarizes the available evidence of vitamin K and vascular calcification in population-based studies and clinic-based studies, with a specific focus on CKD patients.
Z Kardiol. 2001;90 Suppl 3:57-63.
Role of vitamin K and vitamin K-dependent proteins in vascular calcification.
Schurgers LJ, Dissel PE, Spronk HM, Soute BA, Dhore CR, Cleutjens JP, Vermeer C.
OBJECTIVES:
To provide a rational basis for recommended daily allowances (RDA) of dietary phylloquinone (vitamin K1) and menaquinone (vitamin K2) intake that adequately supply extrahepatic (notably vascular) tissue requirements.
BACKGROUND:
Vitamin K has a key function in the synthesis of at least two proteins involved in calcium and bone metabolism, namely osteocalcin and matrix Gla-protein (MGP). MGP was shown to be a strong inhibitor of vascular calcification. Present RDA values for vitamin K are based on the hepatic phylloquinone requirement for coagulation factor synthesis. Accumulating data suggest that extrahepatic tissues such as bone and vessel wall require higher dietary intakes and have a preference for menaquinone rather than for phylloquinone.
METHODS:
Tissue-specific vitamin K consumption under controlled intake was determined in warfarin-treated rats using the vitamin K-quinone/epoxide ratio as a measure for vitamin K consumption. Immunohistochemical analysis of human vascular material was performed using a monoclonal antibody against MGP. The same antibody was used for quantification of MGP levels in serum.
RESULTS:
At least some extrahepatic tissues including the arterial vessel wall have a high preference for accumulating and using menaquinone rather than phylloquinone. Both intima and media sclerosis are associated with high tissue concentrations of MGP, with the most prominent accumulation at the interface between vascular tissue and calcified material. This was consistent with increased concentrations of circulating MGP in subjects with atherosclerosis and diabetes mellitus.
CONCLUSIONS:
This is the first report demonstrating the association between MGP and vascular calcification. The hypothesis is put forward that undercarboxylation of MGP is a risk factor for vascular calcification and that the present RDA values are too low to ensure full carboxylation of MGP.
Am J Clin Nutr. 2009 Jun;89(6):1799-807. doi: 10.3945/ajcn.2008.27338. Epub 2009 Apr 22.
Vitamin K supplementation and progression of coronary artery calcium in older men and women.
Shea MK, O’Donnell CJ, Hoffmann U, Dallal GE, Dawson-Hughes B, Ordovas JM, Price PA, Williamson MK, Booth SL.
BACKGROUND:
Coronary artery calcification (CAC) is an independent predictor of cardiovascular disease. A preventive role for vitamin K in CAC progression has been proposed on the basis of the properties of matrix Gla protein (MGP) as a vitamin K-dependent calcification inhibitor.
OBJECTIVE:
The objective was to determine the effect of phylloquinone (vitamin K1) supplementation on CAC progression in older men and women.
DESIGN:
CAC was measured at baseline and after 3 y of follow-up in 388 healthy men and postmenopausal women; 200 received a multivitamin with 500 microg phylloquinone/d (treatment), and 188 received a multivitamin alone (control).
RESULTS:
In an intention-to-treat analysis, there was no difference in CAC progression between the phylloquinone group and the control group; the mean (+/-SEM) changes in Agatston scores were 27 +/- 6 and 37 +/- 7, respectively. In a subgroup analysis of participants who were > or =85% adherent to supplementation (n = 367), there was less CAC progression in the phylloquinone group than in the control group (P = 0.03). Of those with preexisting CAC (Agatston score > 10), those who received phylloquinone supplements had 6% less progression than did those who received the multivitamin alone (P = 0.04). Phylloquinone-associated decreases in CAC progression were independent of changes in serum MGP. MGP carboxylation status was not determined.
CONCLUSIONS:
Phylloquinone supplementation slows the progression of CAC in healthy older adults with preexisting CAC, independent of its effect on total MGP concentrations. Because our data are hypothesis-generating, further studies are warranted to clarify this mechanism. This trial was registered at clinicaltrials.gov as NCT00183001.
Thromb Res. 2008;122(3):411-7. doi: 10.1016/j.thromres.2007.12.005. Epub 2008 Jan 30.
Effects of the blood coagulation vitamin K as an inhibitor of arterial calcification.
Wallin R, Schurgers L, Wajih N.
INTRODUCTION:
The transformation of smooth muscle cells (VSMCs) in the vessel wall to osteoblast like cells is known to precede arterial calcification which may cause bleeding complications. The vitamin K-dependent protein MGP has been identified as an inhibitor of this process by binding BMP-2, a growth factor known to trigger the transformation. In this study, we determined if the vitamin K-dependent Gla region in MGP by itself can inhibit the growth factor activity of BMP-2 and if menaquinone-4 (MK4) regulates gene expression in VSMCs.
MATERIALS AND METHODS:
A synthetic gamma-carboxyglutamic acid (Gla) containing peptide covering the Gla region in human MGP was used to test its ability to inhibit BMP-2 induced transformation of mouse pro-myoblast C2C12 cells into osteoblasts. MK4 was tested by microarray analysis as a gene regulatory molecule in VSMCs.
RESULTS AND CONCLUSIONS:
The results show that the Gla – but not the Glu-peptide inhibited the transformation which provide evidence that the Gla region in MGP is directly involved in the BMP-2/MGP interaction and emphasizes the importance of the vitamin K-dependent modification of MGP. From the data obtained from the microarray analysis, we focused on two quantitatively altered cDNAs representing proteins known to be associated with vessel wall calcification. DT-diaphorase of the vitamin K-cycle, showed increased gene expression with a 4.8-fold higher specific activity in MK4 treated cells. Osteoprotegrin gene expression was down regulated and osteoprotegrin protein secretion from the MK4 treated cells was lowered to 1.8-fold. These findings suggest that MK4 acts as an anti-calcification component in the vessel wall.
Am J Clin Nutr. 2009 Oct;90(4):889-907. doi: 10.3945/ajcn.2009.27930. Epub 2009 Aug 19.
Vitamin K, an example of triage theory: is micronutrient inadequacy linked to diseases of aging?
McCann JC, Ames BN.
The triage theory posits that some functions of micronutrients (the approximately 40 essential vitamins, minerals, fatty acids, and amino acids) are restricted during shortage and that functions required for short-term survival take precedence over those that are less essential. Insidious changes accumulate as a consequence of restriction, which increases the risk of diseases of aging. For 16 known vitamin K-dependent (VKD) proteins, we evaluated the relative lethality of 11 known mouse knockout mutants to categorize essentiality. Results indicate that 5 VKD proteins that are required for coagulation had critical functions (knockouts were embryonic lethal), whereas the knockouts of 5 less critical VKD proteins [osteocalcin, matrix Gla protein (Mgp), growth arrest specific protein 6, transforming growth factor beta-inducible protein (Tgfbi or betaig-h3), and periostin] survived at least through weaning. The VKD gamma-carboxylation of the 5 essential VKD proteins in the liver and the 5 nonessential proteins in nonhepatic tissues sets up a dichotomy that takes advantage of the preferential distribution of dietary vitamin K1 to the liver to preserve coagulation function when vitamin K1 is limiting. Genetic loss of less critical VKD proteins, dietary vitamin K inadequacy, human polymorphisms or mutations, and vitamin K deficiency induced by chronic anticoagulant (warfarin/coumadin) therapy are all linked to age-associated conditions: bone fragility after estrogen loss (osteocalcin) and arterial calcification linked to cardiovascular disease (Mgp). There is increased spontaneous cancer in Tgfbi mouse knockouts, and knockdown of Tgfbi causes mitotic spindle abnormalities. A triage perspective reinforces recommendations of some experts that much of the population and warfarin/coumadin patients may not receive sufficient vitamin K for optimal function of VKD proteins that are important to maintain long-term health.
Thromb Haemost. 2007 Jul;98(1):120-5.
Vitamin K: the coagulation vitamin that became omnipotent.
Cranenburg EC, Schurgers LJ, Vermeer C.
Vitamin K, discovered in the 1930s, functions as cofactor for the posttranslational carboxylation of glutamate residues. Gammacarboxy glutamic acid (Gla)-residues were first identified in prothrombin and coagulation factors in the 1970s; subsequently, extra-hepatic Gla proteins were described, including osteocalcin and matrix Gla protein (MGP). Impairment of the function of osteocalcin and MGP due to incomplete carboxylation results in an increased risk for developing osteoporosis and vascular calcification, respectively, and is an unexpected side effect of treatment with oral anticoagulants. It is conceivable that other side effects, possible involving growth-arrest-specific gene 6 (Gas6) protein will be identified in forthcoming years. In healthy individuals, substantial fractions of osteocalcin and MGP circulate as incompletely carboxylated species, indicating that the majority of these individuals is subclinically vitamin K-deficient. Potential new application areas for vitamin K are therefore its use in dietary supplements and functional foods for healthy individuals to prevent bone and vascular disease, as well as for patients on oral anticoagulant treatment to offer them protection against coumarin-induced side effects and to reduce diet-induced fluctuations in their INR values.
Eur Heart J. 2011 Oct;32(20):2555-62. doi: 10.1093/eurheartj/ehr226. Epub 2011 Jul 20.
Patients using vitamin K antagonists show increased levels of coronary calcification: an observational study in low-risk atrial fibrillation patients.
Weijs B, Blaauw Y, Rennenberg RJ, Schurgers LJ, Timmermans CC, Pison L, Nieuwlaat R, Hofstra L, Kroon AA, Wildberger J, Crijns HJ.
AIMS:
Vitamin K antagonists (VKA) are currently the most frequently used drug to prevent ischaemic stroke in atrial fibrillation (AF) patients. However, VKA use has been associated with increased vascular calcification. The aim of this study was to investigate the contribution of VKA use to coronary artery calcification in low-risk AF patients.
METHODS AND RESULTS:
A prospective coronary calcium scan was performed in 157 AF patients without significant cardiovascular disease (108 males; mean age 57 ± 9 years). A total of 71 (45%) patients were chronic VKA users. The duration of VKA treatment varied between 6 and 143 months (mean 46 months). No significant differences in clinical characteristics were found between patients on VKA treatment and non-anticoagulated patients. However, median coronary artery calcium scores differed significantly between patients without and patients with VKA treatment [0, inter-quartile range (IQR) 0-40, vs. 29, IQR 0-184; P = 0.001]. Mean coronary calcium scores increased with the duration of VKA use (no VKA: 53 ± 115, 6-60 months on VKA: 90 ± 167, and >60 months on VKA: 236 ± 278; P < 0.001). Multivariable logistic regression analysis revealed that age and VKA treatment were significantly related to increased coronary calcium score.
CONCLUSION:
Patients using VKA show increased levels of coronary calcification. Age and VKA treatment were independently related to increased coronary calcium score.
Blood Rev. 2012 Jul;26(4):155-66. doi: 10.1016/j.blre.2012.03.002. Epub 2012 Apr 18.
Vascular calcification: the price to pay for anticoagulation therapy with vitamin K-antagonists.
Chatrou ML, Winckers K, Hackeng TM, Reutelingsperger CP, Schurgers LJ.
Vitamin K-antagonists (VKA) are the most widely used anti-thrombotic drugs with substantial efficacy in reducing risk of arterial and venous thrombosis. Several lines of evidence indicate, however, that VKA inhibit not only post-translational activation of vitamin K-dependent coagulation factors but also synthesis of functional extra-hepatic vitamin K-dependent proteins thereby eliciting undesired side-effects. Vascular calcification is one of the recently revealed side-effects of VKA. Vascular calcification is an actively regulated process involving vascular cells and a number of vitamin K-dependent proteins. Mechanistic understanding of vascular calcification is essential to improve VKA-based treatments of both thrombotic disorders and atherosclerosis. This review addresses vitamin K-cycle and vitamin K-dependent processes of vascular calcification that are affected by VKA. We conclude that there is a growing need for better understanding of the effects of anticoagulants on vascular calcification and atherosclerosis.
Arterioscler Thromb Vasc Biol. 2000 Feb;20(2):317-27.
Warfarin-induced artery calcification is accelerated by growth and vitamin D.
Price PA, Faus SA, Williamson MK.
The present studies demonstrate that growth and vitamin D treatment enhance the extent of artery calcification in rats given sufficient doses of Warfarin to inhibit gamma-carboxylation of matrix Gla protein, a calcification inhibitor known to be expressed by smooth muscle cells and macrophages in the artery wall. The first series of experiments examined the influence of age and growth status on artery calcification in Warfarin-treated rats. Treatment for 2 weeks with Warfarin caused massive focal calcification of the artery media in 20-day-old rats and less extensive focal calcification in 42-day-old rats. In contrast, no artery calcification could be detected in 10-month-old adult rats even after 4 weeks of Warfarin treatment. To directly examine the importance of growth to Warfarin-induced artery calcification in animals of the same age, 20-day-old rats were fed for 2 weeks either an ad libitum diet or a 6-g/d restricted diet that maintains weight but prevents growth. Concurrent treatment of both dietary groups with Warfarin produced massive focal calcification of the artery media in the ad libitum-fed rats but no detectable artery calcification in the restricted-diet, growth-inhibited group. Although the explanation for the association between artery calcification and growth status cannot be determined from the present study, there was a relationship between higher serum phosphate and susceptibility to artery calcification, with 30% higher levels of serum phosphate in young, ad libitum-fed rats compared with either of the groups that was resistant to Warfarin-induced artery calcification, ie, the 10-month-old rats and the restricted-diet, growth-inhibited young rats. This observation suggests that increased susceptibility to Warfarin-induced artery calcification could be related to higher serum phosphate levels. The second set of experiments examined the possible synergy between vitamin D and Warfarin in artery calcification. High doses of vitamin D are known to cause calcification of the artery media in as little as 3 to 4 days. High doses of the vitamin K antagonist Warfarin are also known to cause calcification of the artery media, but at treatment times of 2 weeks or longer yet not at 1 week. In the current study, we investigated the synergy between these 2 treatments and found that concurrent Warfarin administration dramatically increased the extent of calcification in the media of vitamin D-treated rats at 3 and 4 days. There was a close parallel between the effect of vitamin D dose on artery calcification and the effect of vitamin D dose on the elevation of serum calcium, which suggests that vitamin D may induce artery calcification through its effect on serum calcium. Because Warfarin treatment had no effect on the elevation in serum calcium produced by vitamin D, the synergy between Warfarin and vitamin D is probably best explained by the hypothesis that Warfarin inhibits the activity of matrix Gla protein as a calcification inhibitor. High levels of matrix Gla protein are found at sites of artery calcification in rats treated with vitamin D plus Warfarin, and chemical analysis showed that the protein that accumulated was indeed not gamma-carboxylated. These observations indicate that although the gamma-carboxyglutamate residues of matrix Gla protein are apparently required for its function as a calcification inhibitor, they are not required for its accumulation at calcification sites.
Posted in General.
Comments Off on Vitamin K, Calcification, & Atherosclerosis
– March 3, 2013