Also see:
LED Light Therapy Could Radically Change Our Treatment of Brain Disease
Collection of Ray Peat Quote Blogs by FPS
Collection of FPS Charts
Master List – Ray Peat, PhD Interviews
Protective Glycine
Thyroid peroxidase activity is inhibited by amino acids
Gelatin, Glycine, and Metabolism
Gelatin > Whey
Ray Peat, PhD on Endotoxin
Bowel Toxins Accelerate Aging
Ray Peat, PhD on the Benefits of the Raw Carrot
Protective Cascara Sagrada and Emodin
Fermentable Carbohydrates, Anxiety, Aggression
Protective Bamboo Shoots
Endotoxin-lipoprotein Hypothesis
Endotoxin: Poisoning from the Inside Out
Protection from Endotoxin
How does estrogen enhance endotoxin toxicity? Let me count the ways.
Intestinal Serotonin and Bone Loss
Carbon Dioxide Basics
Comparison: Carbon Dioxide v. Lactic Acid
Carbon Dioxide as an Antioxidant
Bohr Effect and Cells O2 Levels: Healthy vs. Sick People
Comparison: Oxidative Metabolism v. Glycolytic Metabolic
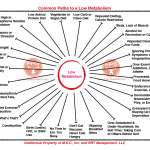
Promoters of Efficient v. Inefficient Metabolism
Altitude Sickness: Therapeutic Effects of Acetazolamide and Carbon Dioxide
Low CO2 in Hypothyroidism
Protective Altitude
Lactate Paradox: High Altitude and Exercise
Protective Carbon Dioxide, Exercise, and Performance
Benefits of Aspirin
Ray Peat, PhD on Aspirin
Sodium Deficiency in Pre-eclampsia
Role of Serotonin in Preeclampsia
“Prostaglandins, platelet activating factor, nitric oxide, peroxidase, lipases, histamine, serotonin, lactate, insulin, intracellular calcium, carbon dioxide, osmolarity, pH, and the redox environment are all relevant to cancer, and are affected systemically and locally by estrogen and progesterone in generally opposing ways.”
“And, obviously, drugs that are intended to increased the effects of nitric oxide (asparagine, zildenafil/Viagra, minoxidil/Rogaine) and acetylcholine (bethanechol, benzpyrinium, etc.) should be avoided.”
“The basic control of blood flow in the brain is the result of the relaxation of the wall of blood vessels in the presence of carbon dioxide, which is produced in proportion to the rate at which oxygen and glucose are being metabolically combined by active cells. In the inability of cells to produce CO2 at a normal rate, nitric oxide synthesis in blood vessels can cause them to dilate. The mechanism of relaxation by NO is very different, however, involving the inhibition of mitochondrial energy production (Barron, et al., 2001). Situations that favor the production and retention of larger amounts of carbon dioxide in the tissues are likely to reduce the basic “tone” of the parasympathetic nervous system, and there is less need for additional vasodilation.”
“Nitric oxide is increasingly seen as an important factor in nerve degeneration (Doherty, 2011). Nitric oxide activates processes (Obukuro, et al., 2013) that can lead to cell death. Inhibition on the production of nitric oxide protects again various kinds of dementia (Sharma & Sharma, 2013, Sharma & Singh, 2013). Brain trauma cases large increase in nitric oxide formation, and blocking its synthesis improves recovery (Huttenmann, et al., 2008); Gahn, et al., 2006).
Organophosphates increase nitric oxide formation, and the protective anticholinergic drugs such as atropine reduce it (Chang, et al., 2001; Kim, et al., 1997). Stress, including fear (Campos., et al., 2013) and isolation (Zlatokovic & Filipovic, 2013) can activate the formation of nitric oxide, and various mediators of inflammation also activate it. The nitric oxide in a person’s exhaled breath can be used to diagnose some diseases, and it probably reflects the level of their emotional well-being.”
“Niacianamide, like progesterone, inhibits the production of nitric oxide, and also like progesterone, it improves recovery from brain injury. (Hoane, et al., 2008).”
“There is a lot of talk about melatonin’s function as an antioxidant, but, like so many other “antioxidants,” melatonin can act as a pro-oxidant at physiologically relevant concentrations; some studies have found that it, like estrogen, increases the activity of the pro-oxidative free radical nitric oxide (which acts like melatonin on pigment cells, causing them to lighten). The promoters of estrogen are also making claims that estrogen is a protective antioxidant, though that isn’t true of physiological concentrations of the estrogens, which can catalyze intense oxidations. The market culture seems to guide most research in these substances.”
“When doctors are talking about diseases of the heart and circulatory system, it’s common for them to say that estrogen is protective, because it causes blood vessels to relax and dilate, improving circulation and preventing hypertension. The fact that estrogen increases the formation of nitric oxide, a vasodilator, is often mentioned as one of its beneficial effects. But in the case of hot flashes, dilation of the blood vessels is exactly the problem, and estrogen is commonly prescribed to prevent the episodic dilation of blood vessels that constitutes the hot flash. Nitric oxide increases in women in association with the menopause (Watanabe, et al., 2000), and it is increased by inflammation, and hot flushes are associated with various mediators of inflammation, but, as far as I can tell, no one has measured the production of nitric oxide during a hot flash. Inhibitors of nitric oxide formation reduce vasodilation during hot flushes (Hubing, et al., 2010).”
“The exhaled breath is being used to diagnose inflammatory lung disease, since so many of the mediators of inflammation are volatile, but systemic diseases such as cancer and arthritis, and relatively minor stress can be detected by changes in the chemicals found in the breath. Polyunsaturated fats and their breakdown products-aldehydes, prostaglandins, isoprostanes, hydrocarbons, and free radicals–and carbon monoxide, nitric oxide, nitrite, and hydrogen peroxide are increased in the breath by most stresses.
Both proline and glycine (which are major amino acids in gelatin) are very protective for the liver, increasing albumin, and stopping oxidative damage.”
“Although fish oil interferes with prostaglandin synthesis, it can contribute to the formation of PAF (Triggiani, et aI., 1990), and other mediators of inflammation, energy suppression, and free radicals, including nitric oxide (Nishimura, et aI., 2000; Hirafuji, et aI., 2002). Since the fish oils are commonly studied by comparing the supplemented animals with “control” animals receiving soy oil, corn oil, or safflower oil, which are strongly pro-inflammatory and broadly toxic, it isn’t surprising that their effects usually seem favorable. But when they are compared with saturated fats (as I mentioned in the “Fats and degeneration” newsletter) or with a fat free diet, their effects are seen to be pro-inflammatory and toxic.”
“Although caffeine, if it’s combined with hypoglycemia and stress, will increase lipolysis and free fatty acids, several of the methylxanthines, including caffeine, theophylline, and pentoxifylline, can protect against capillary leakage, probably by a variety of antiinflammatory actions, including inhibition of nitric oxide synthesis (Bereta, et al., 1994).”
“The unsaturated fats and estrogen contribute to the increased release of serotonin and nitric oxide (NO). Nitric oxide is produced during inflammation, and, like ethane, can be detected in the breath when the lungs are inflamed. Nitric oxide, as a pro-inflammatory free radical, stimulates the peroxidation of the unsaturated fats. Both NO and serotonin inhibit mitochondrial respiration, shifting metabolism toward glycolysis.”
“In women with preeclampsia, there are abnormally high levels of serotonin, nitric oxide, and lipid peroxidation.”
“In women with preeclampsia, there are abnormally high levels of serotonin, nitric oxide, and lipid peroxidation. In a study of more than 3000 women (Clausen, et al., 2001), the consumption of sugar and polyunsaturated fat was strongly associated with the development of preeclampsia. Women who don’t eat enough protein are likely to substitute sugar and fat for the absent protein, so this study is consistent with Brewer’s work, but it’s very important to see that it was polyunsaturated fats, not saturated or monounsaturated fats, that caused the problem. Eclampsia (pregnancy-related seizures) and preeclampsia are caused by oxidative stress, produced by the excessive unstable fats. The increased serotonin and nitric oxide are exactly what would be expected to result from the high consumption of polyunsaturated fats, especially with a deficiency of protein in the diet.”
“Yaffe, et al., in associating depression and osteoporosis with dementia, are arguing that estrogen deficiency is the cause of all three conditions. They offer some hypothetical mechanisms for how estrogen might prevent Alzheimer’s disease. Observing that brain cells die in people with Alzheimer’s disease, they mention that estrogen stimulates “dendritic sprouting” in brain cells, as if that could compensate for the loss of cells (it doesn’t). They observe that estrogen delivers more tryptophan to the brain, increasing the production of serotonin, and that it inhibits the monoamine oxidases and other enzymes that inactivate transmitter substances, increasing the activity of adrenaline, serotonin, and other transmitter substances. They suggest that increased circulation caused by estrogen might protect the brain. Here, Yaffe, et al., have invoked the serotonin myth and other myths, including the nitric oxide myth, to substantiate the estrogen myth.
Serotonin doesn’t “cure depression,” and both serotonin and nitric oxide impair circulation and are toxic to brain cells. Both of them poison mitochondrial respiration. Estrogen increases the viscosity of blood, and impairs circulation and oxygenation in many other ways.”
“Estrogen and PUFA create insulin resistance, and the resulting state of “diabetes” and stress de-energizes tissues, with the mitochondria that are damaged by unsaturated fatty acids, nitric oxide, tumor necrosis factor (TNT), serotonin, etc., failing to meet the tissues’ energy needs. Stress, endotoxinemia, and increased estrogen tend to activate TNF, which has a role in brain degenerative diseases and osteoporosis and multiple organ failure. Much research has focussed on a search for a single substance that is responsible for the inflammatory conditions of Alzheimer’s disease, but inflammation and aging are processes that involve many causes and mediators, with each individual’s history causing variations in the details.”
“Nitric oxide, a third cultic substance along with serotonin and estrogen, is invoked as a normalizer of brain circulation and protector of nerve cells from peroxidation. Whether a substance is an antioxidant or pro-oxidant depends on its environment, and both nitric oxide and estrogen are pro-oxidants, promoters of lipid peroxidation and other forms of cell damage, under a variety of physiological situations.”
“To reverse this process, it’s necessary to avoid doing the things that caused the problem to develop. The accumulation of heavy metals and of the unstable unsaturated fats (linoleic, linolenic, and arachidonic acids) can be slowed or reversed by careful dietary choices. The calorie restricted diets that slow the aging process reduce the accumulation of the unstable fats and the heavy metals. Vitamin E reduces the vascular leakiness and the free radical peroxidation that are so closely involved in fibrosis. Since serotonin and nitric oxide are involved in these processes, they should be minimized by keeping carbon dioxide production high (by optimizing thyroid function), and by eating protein that have a safe balance of the amino acids. Too much arginine increases nitric oxide formation, and too much tryptophan increases serotonin production. Too much glutamic acid, aspartic acid, and cysteine can be directly excitotoxic, and the metabolites of cysteine include proinfiammatory homocysteine, which can disrupt collagen structure.”
“Energy depletion, free-radical generation, and gene mutations are produced by estrogen and by the nitric oxide (NO) promoted by estrogen.”
“Ammonia, like estrogen, promotes the excitotoxic processes, activating the production of nitric oxide (NO), and stimulating the glutamate receptors, sometimes causing seizures, and if prolonged, causing stupor or coma. But it always activates the pituitary, and in other tissues, the production of free radicals causes molecular tissue damage. The stressors produced by estrogen, for example NO and growth hormone, activate the enzyme aromatase, which synthesizes estrogen, in just one of the many vicious circles. Growth hormone tends to increase ammonia levels.
Estrogen is just one of the intrinsic excitatory substances, which are produced by stress, and which participate in self-stimulating loops. Ammonia and nitric oxide are two of the most pervasive endogenous excitants and toxins. NO [nitric oxide] is emerging as an important endogenously-derived neurotoxin” (Dawson and Dawson, 1995).
Ammonia, like nitric oxide, inhibits respiration, and can increase the Crabtree effect (with aerobic glycolysis stimulated by increased glucose, inhibiting respiration). This suggests an important role for it in cancer in general, and especially in liver cancer. In the uncontrolled glycolysis of cancer, ammonia can be used to form amino acids from the lactate and pyruvate produced by glycolysis, supporting growth of the tumor at the expense of the normal tissues that are producing ammonia by protein degradation.”
“Ammonia has also been found to be increased during migraine attacks. I suspect that progesterone’s sometimes dramatic effect on migraine involves ammonia and energy metabolism.
Ammonia disturbs carbon dioxide’s regulation of brain circulation, and when ammonia is “detoxified” into glutamine (though glutamine is still toxic in excess) ATP is consumed, leading to dysregulation of vascular smooth muscle. Progesterone’s ability to stop the local excitation of nerve cells spares ATP. It seems likely that nitric oxide, the production of which is inhibited by progesterone, is also involved in the vasodilation and energy depletion.”
“Lactic acid, produced by splitting glucose to pyruvic acid followed by its reduction, is associated with calcium uptake and nitric oxide production, depletes energy, contributing to cell death.”
“Since the presence of lactate is so commonly considered to be a normal and adaptive response to stress, the shut-down of respiration in the presence of lactate is generally considered to be caused by something else, with lactate being seen as an effect rather than a cause. Nitric oside and calcium exces I have been identified as the main endogenous antirespiratory factors in stress, though free unsaturated fatty acids are clearly involved, too. However, glycolysis and the products of glycolysis, lactate and pyruvate, have been found to have a causal role in the suppression of respiration; it is both a cause and a consequence of the respiratory shutdown, though nitric oxide, calcium, and fatty acids are closely involved.”
“Glycolysis produces both pyruvate and lactate, and excessive pyruvate produces almost the same inhibitory effect as lactate; since the Crabtree effect involves nitric oxide and fatty acids as well as calcium, I think it is reasonable to look for the simplest sort of explanation, instead of trying to experimentally trace all the possible interactions of these substances; a simple physical competition between the products of glycolysis and carbon dioxide, for the binding sites, such as lysine, that would amount to a phase change in the mitochondrion. Glucose, and apparently glycolysis, are required for the production of nitric oxide, as for the accumulation of calcium, at least in some types of cell, and these coordinated changes, which lower energy production, could be produced by a reduction in carbon dioxide, in a physical change even more basic than the energy level represented by ATP The use of Krebs cycle substances in the synthesis of amino acids, and other products, would decrease the formation of CO2, creating a situation in which the system would have two possible states, one, the glycolytic stress state, and the other, the carbon dioxide producing energy-efficient state.”
“But they identified several proteins that estrogen stuck to: ATPase (regulating energy and salt and water), and GAPDH, the rate controlling enzyme of glycolysis. Estrogen activates this enzyme, and physiologically estrogen activates the glycolytic pathway, increasing the production of lactic acid as it shifts metabolism away from mitochondrial oxidation, lowering the cell’s ATP production, and shifts the use of oxygen functions, such as producing nitric oxide, the free radical which is a common mediator for all the harmful forms of radiation, and for oxygen deprivation.”
“Estrogen, like radiation and oxygen deprivation, increases formation of the nitric oxide (NO) free radical, which has so many harmful effects, ranging from damaging DNA to poisoning mitochondria. One of the consequences of increasing NO formation (and estrogen) is the activation of an enzyme (heme oxygenase) which produces carbon monoxide, in the process of breaking down the heme molecule (which is needed for respiratory enzymes, among other essential functions). In previous newsletters I have discussed the reasons for thinking that endogenously produced carbon monoxide could explain the gradual development of cancer, since it stabilizes cells in the primitive anti-respiratory condition.”
“Estrogen, growth hormone, and nitric oxide, which tend to work as a system, along with free fatty acids, all increase the permeability of blood vessels. The leaking of albumin into the urine, which is characteristic of diabetes, is promoted by GH. In diabetes and GH treatment, the basement membrane, the jelly-like material that forms a foundation for capillary cells, is thickened. The reason for this isn’t known, but it could be a compensatory”anti-Ieak” response tending to reduce the leakage of proteins and fats.”
“Carbon monoxide, and other substances such as nitric oxide which also function as respiratory poisons, suppress energy production by the mitochondria, and this activates enzymes which cut DNA molecules, producing either DNA rearrangement, or apoptotic cell death.”
“This would include antiestrogen regimes, antiinflammatory and antihistamine factors (histamine interacts closely with nitric oxide and carbon monoxide), adequate nutrition, carbon dioxide, and specific anti-carbon monoxide therapies (such as light, alcohol, and possibly the minerals which convert porphyrin into compounds that inhibit the production of carbon monoxide), and methods to decrease nitric oxide formation and to restrain cortisol production, since these promote the formation of carbon monoxide. One of the most interesting approaches to inhibiting carbon monoxide production is to use vitamin B12, as hydroxocobalamin, as an antidote to nitric oxide, preventing the nitric oxide from stimulating the formation of heme oxygenase.
Wherever carbon monoxide mediates a biological malfunction, as in acquired immunodeficiency, Alzheimer’s disease, and cancer, vitamin B12 seems to have a place as a detoxicant.”
“Estrogen increases most of the mediators of inflammation, which are generally inhibited by progesterone. Estrogen also shifts many processes toward excitation, and it’s often hard to distinguish the mediators of inflammation from the mediators of excitation. Free polyunsaturated fatty acids, for example, which are increased under the influence of estrogen (or exercise, diabetes, nighttime, aging, histamine, parasympathetic dominance, etc.), produce both inflammation and excitation. Associated with the processes of inflammation and excitation is the tendency of estrogen and other inflammatory mediators, such as nitric oxide and serotonin, to impair mitochondrial respiration. This effect on the cells’ energy production is probably responsible for many of the things that occur in asthma, such as edema and smooth muscle contraction. Acute or chronic interference with mitochondrial respiration can produce a tremendous variety of symptoms, depending on the location, and the degree of the energy deprivation. Exercise, probably acting through some of the same mediators, also impairs mitochondrial respiration.”
“Calcium, which is released into the cytoplasm by the excitotoxins, triggers the release of fatty acids, the activation of nerve and muscle, and the release of a variety of transmitter substances, in a cascade of excitatory processes, but at the same time, it tends to impair mitochondrial metabolism, and progressively tends to accumulate in mitochondria, leading to their calcification death, which is also promoted by the antirespiratory effects of the unsaturated fatty acids and the lipid peroxidation they promote. Iron and calcium both tend to accumulate with aging or stress, and both promote excitatory damage; bicarbonate contributes to keeping iron in its inactive state, and probably has a similar effect against a broad spectrum of excitatory substances. Histamine release, nitric oxide, and carbon monoxide are broadly involved in excitotoxic damage, and carbon dioxide tends to be protective against these, too.”
“The PUFA (especially the omega -3 fatty acids) spontaneously decompose into a variety of toxins, and arachidonate is also enzymically converted into prostaglandins, some of which exacerbate the excitatory damage (pepicelli, et al., 2005); aspirin’s neuroprotective effect (Riepe, et aI., 1997) is probably partly caused by inhibiting prostaglandin synthesis. Besides the prostaglandins, other mediators of inflammation including nitric oxide and interleukins are produced by excessive excitation, as cells lose their ability to retain magnesium, and to control excitatory intracellular calcium.
Nitric oxide, associated with unbalanced excitation, is involved in the nerve damage of epilepsy, amyotrophic lateral sclerosis, Parkinson’s disease, Alzheimer’s disease, and Huntington’s disease. An energy deficit increases excitation and cellular calcium uptake, increasing nitric oxide synthesis (Schulz, et aI., 1997). Nitric oxide increases the ratio of glutamate to GABA (“the excitotoxicity index”), (Demchenko & Piantadosi, 2006), while lowering mitochondrial energy production.
The PUFA increase the susceptibility to excessive serotonin in the nervous system. One of the functions of the GABA system is to inhibit serotonergic nerves (Calogero, et aI., 1988; Kaura, et aI., 2007). Eating a diet with a very low tryptophan content, and lacking PUFA, can support that function of the GABA system. The tea amino acid, theanine, suppresses serotonin by supporting the effects of GABA. Three of the major types of antidepressant also protect against glutamate/aspartate-induced nitric oxide formation and nerve cell damage (Li, et. al., 2006).”
“It is antagonistic to the GABA system, and promotes the action of excitatory transmitters, and increases formation of nitric oxide and prostaglandins. In cancers that are promoted by estrogen, GABA, like progesterone, inhibits cell division. It is an antiproliferative agent in normal tissues, too, opposing estrogen’s effects and supporting progesterone’s.”
“Stress increases nitric oxide, and an excess of that poisons mitochondrial energy production, making stress worse. The right amount of coffee inhibits nitric oxide and so improves energy efficiency. Nitric oxide increases parathyroid hormone and aldosterone, which increase blood pressure. Vitamin D and vitamin K lower those.”
“Bacterial endotoxin increases serotonin release from the intestine, and increases its synthesis in the brain (Nolan, et al., 2000) and liver (Bado, 1983). It also stimulates its release from platelets, and reduces the lungs’ ability to destroy it. The formation of serotonin in the intestine is also stimulated by the lactate, propionate and butyrate that are formed by bacteria fermenting fiber and starch, but these bacteria also produce endotoxin. The inflammation-producing effects of lactate, serotonin, and endotoxin are overlapping, additive, and sometimes synergistic, along with histamine, nitric oxide, bradykinin, and the cytokines.”
“Chronically elevated cortisol is commonly seen in depressed people, but giving a supplement of cortisol is effective in relieving depression. Both cortisol and the pituitary corticotropic hormone that stimulates its production, ACTH, have some antidepressant effects, and they inhibit the hypothalamic corticotropin release honnone, CRH. CRH is more directly associated with depression than cortisol is, and it by itself activates many inflammatory processes, including the release of histamine, cytokines, and nitric oxide. CRH is promoted in the hypothalamus (and in many other tissues) by inflammation, endotoxin, serotonin, interleukins, and prostaglandins, but also by the perception of unavoidable difficulties.”
“A localized stress or irritation at first produces vasodilation that increases the delivery of blood to the tissues, allowing them to compensate for the stress by producing more energy. Some of the agents that produce vasodilation also reduce oxygen consumption (nitric oxide, for example), helping to restore a normal oxygen tension to the tissue. Hypoxia itself (produced by factors other than irritation) can induce vasodilation, and if prolonged sufficiently, tends to produce neovascularization and fibrosis.
Sensitivity to the harmful effects of light can be increased by some drugs and by excess porphyrins produced in the body (and by the porphyrin precursor, delta-amino levulinic acid), leading to rosacea, so those factors should be considered, but too often alcohol (which can cause porphyrin to increase) is blamed for rosacea and rhinophyma, without justification. There are many ways in which poor health can increase light sensitivity. Some types of excitation produced by metabolites (or by the failure of inhibitory metabolites) can produce vasodilation, involving the release of nitric oxide (Cardenas, et al., 2000), setting off a series of potentially pathological reactions, including fibrosis. The nitric oxide increases glycolysis while lowering energy production. The excitatory metabolite glutamate, and nitric oxide, are both inhibited by aspirin (Moro, et al., 2000).”
“The excess excitation that produces nitric oxide and lactic acid lowers the energy production of vascular cells, possibly enough to lower their contractile ability (Geng, et al., 1992), causing vasodilation. When flushing is caused by a mismatch between energy supply and energy demand, caffeine can decrease the vasodilation (Eikvar & Kirkebeen, 1998), but when vasodilation is caused more physiologically by carbon dioxide, caffeine doesn’t have that effect (Meno, et al., 2005). In a study in which drinking hot water or coffee was compared with drinking room temperature coffee or caffeine, it was found that the hot liquids caused flushing, but cool coffee and caffeine didn’t.”
“Estrogen’s most immediate effect on cells is to alter their oxidative metabolism. It promotes the formation of lactic acid. In the long run, it increases the nutritional requirements for the B vitamins, as well as for other vitamins. It also increases the formation of aminolevulinic acid, a precursor of porphyrin, and increases the risk of excess porphyrin increasing light sensitivity. Both aminolevulinic acid and excess porphyrins are toxic to mitochondria, apart from their photosensitizing actions. Nitric oxide, glutamate, and cortisol all tend to be increased by estrogen.
Veins and capillaries are highly sensitive to estrogen, and women are more likely than men to have varicose veins, spider veins, leaky capillaries, and other vascular problems besides rosacea. Estrogen can promote angioneogenesis by a variety of mechanisms, including nitric oxide (Johnson, et al., 2006). “Estrogens potentiate corticosteroid effects on the skin such as striae, telangiectasiae, and rosacea dermatitis” (Zaun, 1981). Early forms of oral contraceptives, high in estrogen, were found to increase acne rosacea more than three-fold (prenen & Ledoux-Corbusier, 1971).
Lactic acid, produced under the influence of estrogen, nitric oxide, or other problems of energy formation, besides causing vasodilation, also stimulates the growth of fibroblasts. Oxygen deprivation, or damage to mitochondria, will increase lactic acid formation, and so it will immediately cause vasodilation, and if the problem is prolonged, new blood vessels will grow, and fibrous connective tissue will increase. Estrogen stimulates collagen synthesis, and it has been associated with a variety of inflammatory and fibrotic conditions (for example, Cutolo, et al., 2003. Payne, et al., 2006, suggest the use of the anti-estrogen, tamoxifen, to treat rhinophyma.)”
“Lactate, glutamate, ammonium, nitric oxide, quinolinate, estrogen, histamine, aminolevulinate, porphyrin, ultraviolet light, polyunsaturated fatty acids and endotoxin contribute to excitatory and excitotoxic processes, vasodilation, angioneogenesis, and fibrosis.”
“PTH (like estrogen) causes mast cells to release promoters of inflammation, including histamine and serotonin. Serotonin and nitric oxide contribute to increasing PTH secretion.”
“Multiple sclerosis relapses essentially occur at times of high PTH, and remissions consistently occur at times of low PTH (Soilu-Hfuminen, et al., 2008). PTH increases the activity of nitric oxide synthase, and nitric oxide is a factor in the vascular leakiness that is so important in MS.”
“Substances such as PTH, nitric oxide, serotonin, cortisol, aldosterone, estrogen, thyroid
stimulating hormone, and prolactin have regulatory and adaptive functions that are essential, but that ideally should act only intermittently, producing changes that are needed momentarily. When the environment is too stressful, or when nutrition isn’t adequate, the organism may be unable to mobilize the opposing and complementary substances to stop their actions.”
“Endotoxin and estrogen interact in many interesting and potentially deadly ways. Both of them activate many of the same alarm systems, including phospholipases, nitric oxide synthase, tumor necrosis factor (TNF), interleukins (including IL-6, according to Bengtsson, et aI., 2004), and the enzymes that form prostaglandins from polyunsaturated fatty acids. Estrogen makes the toxic-mediator-producing cells in the liver (Kupffer cells) hypersensitive to LPS–15 times more sensitive than normal (Ikejima, et a!., 1998).”
“Estrogen (like endotoxin) activates nuclear factor kappa-B (Shyamala and Guiot, 1992; Hamilton, et a!., 2003), which activates cells to produce TNF, nitric oxide, prostaglandins, and interleukins. A long series of observations have indicated that estrogen’s main effects begin with redox changes in the mitochondria, and recent evidence (Felty and Roy, 2005) shows that oxidative free radicals produced in the mitochondria by estrogen induce NF kappa-B. Old age is associated with increased activity of NF kappa-B.”
“Nitric oxide, which is promoted by resveratrol, according to numerous publications (Klinge, et al., 2008; Gresele, et al. 2008; Gan, et al., 2009), and estrogens (acting partly through nitric oxide), including some phytoestrogens, cause chromosomal damage (Banerjee, et al., 1994; Kulling, et al., 1999) which contributes to cancer and possibly to birth defects. Nitric oxide has been proposed to be a major factor in causing the degenerative diseases of aging.”
“Niacinamide protects mitochondrial respiration from many of the age-related factors that can damage mitochondria and decrease energy production. Lipopolysaccharide, the bacterial endotoxin, increases the production of the free radical nitric oxide, leading to the secretion of inflammatory mediators and the suppression of energy production by the mitochondria. These effects are blocked by niacinamide (Fukuzawa, et al., 1997). Calorie restriction also protects mitochondrial respiration, in yeasts (Lin, et al., 2002) and rats (Broderick, et al., 2002)”
“In an experiment with human keratinocytes in vitro, resveratrol had the opposite effect, reducing their ability to divide (Blander, et al., 2009). By the definitions of “aging” used by the advocates of the rate-of-living theory, this experiment suggests that resveratrol causes premature aging. Estrogen has a similar effect on keratinocytes. Resveratrol, nitric oxide, and estrogen, unlike niacinamide, suppress mitochondrial respiration. Resveratrol inhibits the formation of progesterone (Chen, et al., 2007), which is synthesized in mitochondria.”
“One factor involved in the increased production of TSH in hypothyroidism is that the low metabolic rate allows estrogen to accumulate, leading to increased serotonin production. Serotonin stimulates both TSH and prolactin. Serotonin and prolactin both happen to cause bone loss. They increase nitric oxide, which inhibits mitochondrial respiration. Serotonin increases a cytokine, osteoprotegerin, that inhibits osteoclasts, reducing bone turnover. However, serotonin’s other antimetabolic effects outweigh that effect, and it is a major factor in causing osteoporosis. The antimetabolic factors that slow the rate of living also slow the rate of renewal, and on balance lead to tissue atrophy, fibrosis, inflammation, and degeneration. Several decades after estrogen-induced prolactin might have been recognized as a cause of bone loss in aging, a few people are mentioning the mechanism in specific situations (Homer, 2009; Homer, et al., 2007).”
“In the presence of bacterial endotoxin, respiratory energy production fails in the cells lining the intestine. Nitric oxide is probably the main mediator of this effect.”
“Since the cells that form the barrier begin to form regulatory substances such as nitric oxide when they are exposed to endotoxin, it is clear that major metabolic and energetic changes coincide in the cell with the observed leakiness. Permeability varies with the nature of the substance, its oil and water solubility, and the direction of its movement, arguing clearly that it isn’t a matter of mere holes between cells.
Besides endotoxin, estrogen, vibrational injury, radiation, aging, cold, and hypoosmolarity, increase NO synthesis and release, and increase cellular permeabilities throughout the body.
Estrogen excess (relative to progesterone and androgens), as in pregnancy, stress, and aging, reduces intestinal motility, probably by increasing nitric oxide production. The anthraquinones inhibit the formation of nitric oxide, which is constantly being promoted by endotoxin.”
“Emodin inhibits the formation of nitric oxide, increases mitochondrial respiration, inhibits angiogenesis and invasiveness, inhibits fatty acid synthase (Zhang, et al., 2002), inhibits HER-2 neu and tyrosine phosphorylases (Zhang, et al., 1995, 1999), and promotes cellular differentiation in cancer cells (Zhang, et al., 1995). The anthraquinones, like other antiinflammatory substances, reduce leakage from blood vessels, but they also reduce the absorption of water from the intestine. Reduced water absorption can be seen in a slight
shrinkage of cells in certain circumstances, and is probably related to their promotion of cellular differentiation.”
“Zelnorm was said to “act like serotonin.” Serotonin slows metabolism, reduces oxygen consumption, and increases free radicals such as superoxide and nitric oxide; the production of reactive oxygen species is probably an essential part of its normal function. Emodin has an opposing effect, increasing the metabolic rate. It increases mitochondrial oxygen consumption and ATP synthesis, while decreasing oxidative damage (Du and Ko, 2005, 2006; Huang, et al., 1995).”
“When destabilizing factors are transmitted from cells that were damaged, for example by irradiation, to other cells that weren’t exposed to the radiation, but which then undergo changes similar to those of the exposed cells, these changes are called “bystander effects.” Besides being transmitted from one part of the body to another, for example from the head to the reproductive organs, these effects can even be transmitted from one animal to another, for example from fish exposed to radiation to other fish which enter water after the exposed fish have been in it (Mothersill, et aI., 2007). Serotonin has been identified as one of the substances transmitting the effect (poon, et aI., 2007). In some situations, the transmitted factors include nitric oxide and “persistent” free radicals (Harada, et al. 2008).”
“Lactic acid activates the other major mediators of inflammation, including prostaglandins (made from PDFA), free fatty acids (including arachidonate, that forms prostaglandins; Schoonderwoerd, et al., 1989), nitric oxide, carbon monoxide, proteolytic enzymes that degrade the extracellular matrix, TNF (Jensen, et al.,· 1990), hypoxia inducible factor (Lu, et al., 2002; McFate, et al., 2008), interferon, and interleukins. Arachidonic acid itself can increase lactate production (Meroni, et aI., 2003). TNFalpha and interferon gamma activate lactic acid production by increasing prostaglandins (Taylor, et al., 1992).
Most of the present information about cancer cells’ behavior, such as reactions to radiation and chemical toxins, has been based on the study of cells in culture dishes. For more than 70 years, it was generally believed that radiation caused mutations and cancer by directly modifying the cells’ genetic material. Then, it was discovered that fresh cells that were added to a dish of irradiated cells also developed mutations. The radiation causes cells to emit excitatory, inflammatory, substances such as serotonin and nitric oxide, which injure the cells that are later put near them.”
“We are susceptible to many things that interfere with energy production-the substitution of iron for copper in the respiratory enzyme, the absorption of endotoxin, the accumulation of PUFA, a deficiency of thyroid hormone, the formation of increased amounts of nitric oxide, serotonin, and histamine, etc. Different environments will condition the way the defensive mechanisms of inflammation are produced.”
“When it was discovered that the endothelial relaxing factor was nitric oxide, a new drug business came into being. Nitroglycerine had been in use for decades to open blood vessels, and, ignoring the role of nitrite vasodilators in the acquired immunodeficiency syndrome, new drugs were developed to increase the production of nitric oxide. The estrogen industry began directing research toward the idea that estrogen works through nitric oxide to “improve” the function of blood vessels and the heart.”
“More recently, it has been discovered that progesterone inhibits the expression of the enzyme nitric oxide synthase while estrogen stimulates its expression. At the time of ovulation, when estrogen is high, a woman breathes out 50% more nitric oxide (“NO”) than’ men do, but at other times, under the influence of increased progesterone and thyroid, and reduced estrogen, women exhale much less NO than men do. (Nitric oxide is a free radical, and it decomposes’ into other toxic compounds, including the free radical peroxyrutnle} which damages cells, including the blood vessels. brain, and heart. Carbon dioxide tends to inhibit the production of peioxynitrile.)”
If nitric oxide produced under the influence of estrogen were important in preventing cardiovascular disease, then men’s larger production of nitric oxide would give them greater protection than women have.
From more realistic perspectives, nitric oxide is being considered as a cause of aging, especially brain aging. Nitric oxide interacts with unsaturated fats to reduce oxygen use, damage mitochondria, and cause edema.”
“Progesterone’s effects are antagonistic to estrogen’s: Progesterone decreases the formation of nitric oxide, decreasing edema; it strengthens the heart beat, by improving venous return and increasing stroke volume, but at the same time it reduces peripheral resistance by relaxing arteries (by inhibiting calcium entry but also by other effects and independently of the endothelium) and decreasing edematous swelling.
The effects of progesterone on the heart and blood vessels are paralleled by those of carbon dioxide: Increased carbon dioxide increases perfusion of the heart muscle, increases its stroke volume, and reduces peripheral resistance. The physical and chemical properties of carbon dioxide that I have written about previously include protective anti-excitatory and energy-sustaining functions that explain these effects. Since these effects have been known for many years, I think it is obvious that the obsessive interest in explaining these functions in terms of other molecules, such as nitric oxide, is motivated by the desire for new drugs, not by a desire to understand the physiology with which the researchers are pretending to deal.”
“An extracellular phosphorylated fructose metabolite, diphosphoglycerate, has an essential regulatory effect in the blood; another fructose metabolite, fructose diphosphate, can reduce mast cell histamine release and protect against oxidative and hypoxic injury and endotoxic shock, and it reduces the expression of the inflammation mediators TNF -alpha, I L-6, nitric oxide synthase, and the activation of NF-kappaB, among other protective effects, and its therapeutic value is known, but its relation to dietary sugars hasn’t been investigated.”
“Besides the direct effects of endotoxin and fatty acids, endotoxin’s activation of prostaglandins and nitric oxide contribute to the metabolic shift toward inflammation and away from efficient oxidation of glucose.”