Carbon dioxide (CO2) is the key player in O2 transport due to 1) vasodilation and 2) the the Bohr effect (or the Bohr law). The Bohr effect explains oxygen release in capillaries or why red blood cells unload oxygen in tissues. The Bohr effect was first described in 1904 by the Danish physiologist Christian Bohr (father of famous physicist Niels Bohr). Christian Bohr stated that at lower pH (more acidic environment, e.g., in tissues), hemoglobin will bind to oxygen with less affinity. Since carbon dioxide is in direct equilibrium with the concentration of protons in the blood, increasing blood carbon dioxide content causes a decrease in pH, which leads to a decrease in affinity for oxygen by hemoglobin (and easier oxygen release in capillaries).
The description of this physiological law can be found in standard physiological textbooks. Modern studies in this area are devoted to more advanced topics (e.g., Braumann et al, 1982; Böning et al, 1975; Bucci et al, 1985; Carter et al, 1985; diBella et al, 1986; Dzhagarov et al, 1996; Grant et al, 1982; Grubb et al, 1979; 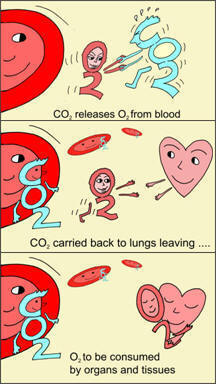 Gersonde et al, 1986; Hlastala & Woodson, 1983; Jensen, 2004; Kister et al, 1988; Kobayashi et al, 1989; Lapennas, 1983; Matthew et al, 1979; Meyer et al, 1978; Tyuma, 1984; Winslow et al, 1985). It is the central proposition of this law that oxygen affinity to hemoglobin depends on absolute CO2 concentrations and reduced CO2 values decrease cells oxygen content.
Gersonde et al, 1986; Hlastala & Woodson, 1983; Jensen, 2004; Kister et al, 1988; Kobayashi et al, 1989; Lapennas, 1983; Matthew et al, 1979; Meyer et al, 1978; Tyuma, 1984; Winslow et al, 1985). It is the central proposition of this law that oxygen affinity to hemoglobin depends on absolute CO2 concentrations and reduced CO2 values decrease cells oxygen content.
What is the Bohr effect in simple terms?
As we know, oxygen is transported in blood by hemoglobin cells. How do these red blood cells know where to release more oxygen and where less? Or why do they unload more oxygen at all? Why is O2 released in tissues? The hemoglobin cells sense higher concentrations of CO2 in tissues and release oxygen in such places.
Conclusion. More oxygen is released in those tissues
that have higher absolute and/or relative CO2 values.
This is true for healthy people who have normal breathing pattern. What about person with chronic diseases?
Minute ventilation rates (chronic diseases)
| Condition | Minute ventilation |
Number of people |
All references or click below for abstracts |
| Normal breathing | 6 L/min | – | Medical textbooks |
| Healthy Subjects | 6-7 L/min | >400 | Results of 14 studies |
| Heart disease | 15 (±4) L/min | 22 | Dimopoulou et al, 2001 |
| Heart disease | 16 (±2) L/min | 11 | Johnson et al, 2000 |
| Heart disease | 12 (±3) L/min | 132 | Fanfulla et al, 1998 |
| Heart disease | 15 (±4) L/min | 55 | Clark et al, 1997 |
| Heart disease | 13 (±4) L/min | 15 | Banning et al, 1995 |
| Heart disease | 15 (±4) L/min | 88 | Clark et al, 1995 |
| Heart disease | 14 (±2) L/min | 30 | Buller et al, 1990 |
| Heart disease | 16 (±6) L/min | 20 | Elborn et al, 1990 |
| Pulm hypertension | 12 (±2) L/min | 11 | D’Alonzo et al, 1987 |
| Cancer | 12 (±2) L/min | 40 | Travers et al, 2008 |
| Diabetes | 12-17 L/min | 26 | Bottini et al, 2003 |
| Diabetes | 15 (±2) L/min | 45 | Tantucci et al, 2001 |
| Diabetes | 12 (±2) L/min | 8 | Mancini et al, 1999 |
| Diabetes | 10-20 L/min | 28 | Tantucci et al, 1997 |
| Diabetes | 13 (±2) L/min | 20 | Tantucci et al, 1996 |
| Asthma | 13 (±2) L/min | 16 | Chalupa et al, 2004 |
| Asthma | 15 L/min | 8 | Johnson et al, 1995 |
| Asthma | 14 (±6) L/min | 39 | Bowler et al, 1998 |
| Asthma | 13 (±4) L/min | 17 | Kassabian et al, 1982 |
| Asthma | 12 L/min | 101 | McFadden & Lyons, 1968 |
| COPD | 14 (±2) L/min | 12 | Palange et al, 2001 |
| COPD | 12 (±2) L/min | 10 | Sinderby et al, 2001 |
| COPD | 14 L/min | 3 | Stulbarg et al, 2001 |
| Sleep apnea | 15 (±3) L/min | 20 | Radwan et al, 2001 |
| Liver cirrhosis | 11-18 L/min | 24 | Epstein et al, 1998 |
| Hyperthyroidism | 15 (±1) L/min | 42 | Kahaly, 1998 |
| Cystic fibrosis | 15 L/min | 15 | Fauroux et al, 2006 |
| Cystic fibrosis | 10 L/min | 11 | Browning et al, 1990 |
| Cystic fibrosis* | 10 L/min | 10 | Ward et al, 1999 |
| CF and diabetes* | 10 L/min | 7 | Ward et al, 1999 |
| Cystic fibrosis | 16 L/min | 7 | Dodd et al, 2006 |
| Cystic fibrosis | 18 L/min | 9 | McKone et al, 2005 |
| Cystic fibrosis* | 13 (±2) L/min | 10 | Bell et al, 1996 |
| Cystic fibrosis | 11-14 L/min | 6 | Tepper et al, 1983 |
| Epilepsy | 13 L/min | 12 | Esquivel et al, 1991 |
| CHV | 13 (±2) L/min | 134 | Han et al, 1997 |
| Panic disorder | 12 (±5) L/min | 12 | Pain et al, 1991 |
| Bipolar disorder | 11 (±2) L/min | 16 | MacKinnon et al, 2007 |
| Dystrophia myotonica | 16 (±4) L/min | 12 | Clague et al, 1994 |
Overbreathing or hyperventilation in the sick (with exception for those who have problems with lungs and ventilation-perfusion mismatch) causes hypocapnia or reduced CO2 tissue tension in the lungs and arterial blood (ventilation-perfusion mismatch is not a common finding in the sick). This leads to hampered oxygen release and reduced cells oxygen tension (Aarnoudse et al, 1981; Monday & Tétreault, 1980; Gottstein et al, 1976).
Hence, if absolute CO2 concentration is low (see the picture of the right side), O2 molecules are stuck with red blood cells. (Scientists call this effect “increased oxygen affinity to hemoglobin”). Hence, CO2 deficiency (hypocapnia) leads to hypoxia or cells oxygen levels (the suppressed Bohr effect). The more we breathe at rest, the less the amount of available oxygen in the cells of vital organs, like brain, heart, liver, kidneys, etc.
Hemoglobin cells in normal blood are about 98% saturated with O2. When we hyperventilate this number is about the same (in best case, since transition to costal or chest breathing reduces arterial blood O2 levels), but without CO2, this oxygen is tightly bound with red blood cells and cannot get into the tissues in required amounts. Hence, now we know one of the causes why heavy breathing reduces cell oxygen level of all vital organs.
 The Bohr effect is crucial for our survival. Why? During each moment of our lives, some organs and tissues work harder and produce more CO2. These additional CO2 concentrations are sensed by the hemoglobin cells and cause them to release more O2 in those places where it is most required. This is a smart self-regulating mechanism for efficient cells oxygen transport.
The Bohr effect is crucial for our survival. Why? During each moment of our lives, some organs and tissues work harder and produce more CO2. These additional CO2 concentrations are sensed by the hemoglobin cells and cause them to release more O2 in those places where it is most required. This is a smart self-regulating mechanism for efficient cells oxygen transport.
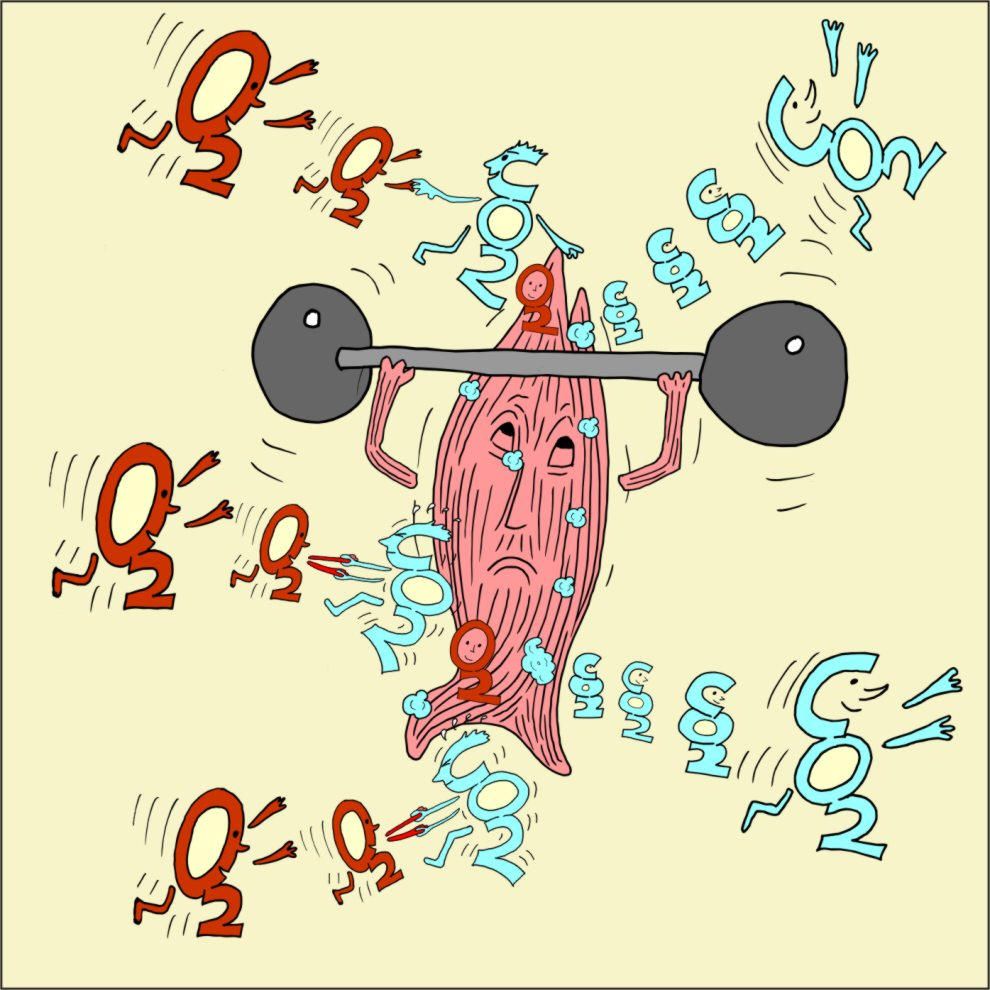
Bohr effect and physical exercise
For example, without the Bohr effect, you could not walk or run for even 3-5 minutes. Why? In normal conditions, due to the Bohr effect, more O2 is released in those muscles, which generate more CO2. Hence, these muscles can continue to work with the same high rate.
However, sick people have reduced CO2 blood values. Hence, they are likely to experience symptoms of chronic fatigue due to tissue hypoxia (low cells oxygen levels).
“But even as early as 1885, Miescher (Swiss physiologist) inspired by the insight of genius wrote: “Over the O2 supply of the body, CO2 spreads its protecting wings” Yandell Henderson (1873-1944), in Henderson Y, Carbon dioxide, in Cyclopedia of Medicine, ed. by HH Young, Philadelphia, FA Davis, 1940.
Here is YouTube video that considers the Bohr effect and explains the mechanism why overbreathing decreases cells oxygen level.
Another web page related to oxygen transport and cell oxygenation: Vasodilation (expansion of arteries and arterioles due to higher CO2 values) or why breathing less improves perfusion and oxygenation of all vital organs.
You can read medical research abstract devoted to the Bohr effect and role of CO2 in cells O2 delivery.
References (abstracts are below)
Aarnoudse JG, Oeseburg B, Kwant G, Zwart A, Zijlstra WG, Huisjes HJ, Influence of variations in pH and PCO2 on scalp tissue oxygen tension and carotid arterial oxygen tension in the fetal lamb, Biol Neonate 1981; 40(5-6): p. 252-263.
Braumann KM, Böning D, Trost F, Bohr effect and slope of the oxygen dissociation curve after physical training, J Appl Physiol. 1982 Jun; 52(6): p. 1524-1529.
Böning D, Schwiegart U, Tibes U, Hemmer B, Influences of exercise and endurance training on the oxygen dissociation curve of blood under in vivo and in vitro conditions, Eur J Appl Physiol Occup Physiol. 1975; 34(1): p. 1-10.
Bucci E, Fronticelli C, Anion Bohr effect of human hemoglobin, Biochemistry. 1985 Jan 15; 24(2): p. 371-376.
Carter AM, Grønlund J, Contribution of the Bohr effect to the fall in fetal PO2 caused by maternal alkalosis, J Perinat Med. 1985; 13(4): p.185-191.
diBella G, Scandariato G, Suriano O, Rizzo A, Oxygen affinity and Bohr effect responses to 2,3-diphosphoglycerate in equine and human blood, Res Vet Sci. 1996 May; 60(3): p. 272-275.
Dzhagarov BM, Kruk NN, The alkaline Bohr effect: regulation of O2 binding with triliganded hemoglobin Hb(O2)3 [Article in Russian] Biofizika. 1996 May-Jun; 41(3): p. 606-612.
Gersonde K, Sick H, Overkamp M, Smith KM, Parish DW, Bohr effect in monomeric insect haemoglobins controlled by O2 off-rate and modulated by haem-rotational disorder, Eur J Biochem. 1986 Jun 2; 157(2): p. 393-404.
Grant BJ, Influence of Bohr-Haldane effect on steady-state gas exchange, J Appl Physiol. 1982 May; 52(5): p. 1330-1337.
Grubb B, Jones JH, Schmidt-Nielsen K, Avian cerebral blood flow: influence of the Bohr effect on oxygen supply, Am J Physiol. 1979 May; 236(5): p. H744-749.
Gottstein U, Zahn U, Held K, Gabriel FH, Textor T, Berghoff W, Effect of hyperventilation on cerebral blood flow and metabolism in man; continuous monitoring of arterio-cerebral venous glucose differences (author’s transl) [Article in German], Klin Wochenschr. 1976 Apr 15; 54(8): p. 373-381.
Hlastala MP, Woodson RD, Bohr effect data for blood gas calculations, J Appl Physiol. 1983 Sep; 55(3): p. 1002-1007.
Jensen FB, Red blood cell pH, the Bohr effect, and other oxygenation-linked phenomena in blood O2 and CO2 transport, Acta Physiol Scand. 2004 Nov; 182(3): p. 215-227.
Kister J, Marden MC, Bohn B, Poyart C, Functional properties of hemoglobin in human red cells: II. Determination of the Bohr effect, Respir Physiol. 1988 Sep; 73(3): p. 363-378.
Kobayashi H, Pelster B, Piiper J, Scheid P, Significance of the Bohr effect for body oxygen level in a model with counter-current blood flow, Respir Physiol. 1989 Jun; 76(3): p. 277-288.
Lapennas GN, The magnitude of the Bohr coefficient: optimal for oxygen delivery, Respir Physiol. 1983 Nov; 54(2): p.161-172.
Matthew JB, Hanania GI, Gurd FR, Electrostatic effects in hemoglobin: Bohr effect and ionic strength dependence of individual groups, Biochemistry. 1979 May 15; 18(10): p.1928-1936.
Meyer M, Holle JP, Scheid P, Bohr effect induced by CO2 and fixed acid at various levels of O2 saturation in duck blood, Pflugers Arch. 1978 Sep 29; 376(3): p. 237-240.
Monday LA, Tétreault L, Hyperventilation and vertigo, Laryngoscope 1980 Jun; 90(6 Pt 1): p.1003-1010.
Tyuma I, The Bohr effect and the Haldane effect in human hemoglobin, Jpn J Physiol. 1984; 34(2): p.205-216.
Winslow RM, Monge C, Winslow NJ, Gibson CG, Whittembury J, Normal whole blood Bohr effect in Peruvian natives of high altitude, Respir Physiol. 1985 Aug; 61(2): p. 197-208.
http://www.normalbreathing.com/CO2-bohr-effect.php
